- I. Core Summary and Future Positioning: Key Takeaways from 2026 Bio International Convention
- II. The First Major Strategic Transformation at 2026 Bio International Convention: From "In Vitro Diagnostics (IVD)" to "Actionable Intelligence"
- III. The Second Major Strategic Transformation Highlighted at 2026 Bio International Convention: Platformization and Democratization of Precision Medicine
- IV. Third Strategic Transformation Unveiled at 2026 Bio International Convention: Global Reshaping and Regional Focus of Industrial Chains
- V. Practical Action Checklist for 2026 Bio International Convention Attendees and Industry Observers
- VI. Conclusion and Long-Term Outlook: Charting the Course Post-2026 Bio International Convention
I. Core Summary and Future Positioning: Key Takeaways from 2026 Bio International Convention
1.1 A Captivating Opening: Medlab 2026 Witnesses a Disruptive Turning Point in Middle Eastern Laboratory Medicine
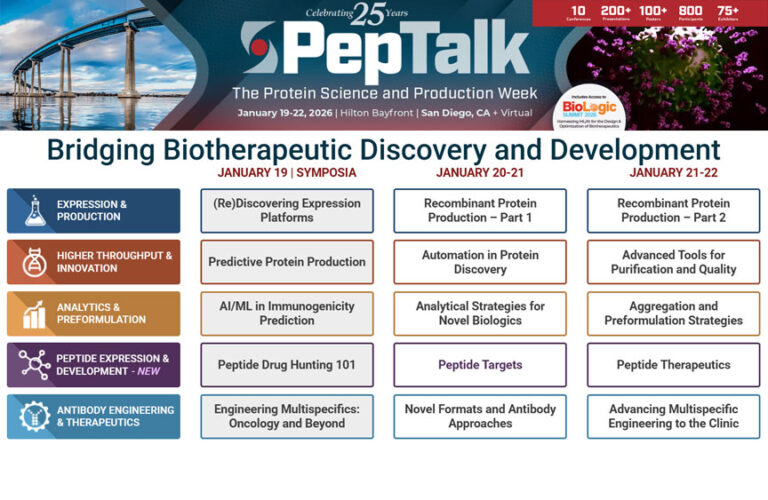
In the 2026 global healthcare landscape, Medlab Middle East—synergizing with the 2026 Bio International Convention—transcends its origins as a regional trade exhibition, evolving into a strategic global hub for laboratory medicine. With attendance surpassing 30,000+ in 2024, Medlab 2026, alongside the 2026 Bio International Convention, will mark the Middle East’s structural shift from a “consumer of high-end medical equipment” to a “pioneer in life sciences innovation”. For global IVD and precision medicine decision-makers, these two landmark events represent a pivotal moment to redefine growth trajectories for the next five years.
For years, the global market’s perception of the Middle East’s healthcare sector has been limited to its robust end-consumer spending power and capital-intensive private healthcare services, often assuming a lack of indigenous industrial chain support. But if you attended the 2024 Medlab exhibition, that impression would have been completely shattered.Last year, I specifically flew to Dubai to explore the event. Upon entering the exhibition hall, I was immediately struck: among the 30,000 attendees, alongside massive booths from global healthcare giants like Siemens and Roche, numerous Middle Eastern companies showcased their independently developed IVD devices and gene sequencing kits.From hospital procurement teams in Nigeria to European tech startups and Chinese nucleic acid drug companies, people of diverse backgrounds and accents crowded around booths exchanging ideas. This trend of “global resources converging on the Middle East” is undeniable, with its industrial magnetism experiencing explosive growth.
Previously, the Middle Eastern healthcare market functioned more like an “end-consumer market”—spending money on advanced equipment and top-tier doctors to address local high-end medical needs.But now, as evident from the evolution of the Medlab exhibition, the Middle East is proactively building an “industrial chain ecosystem”: at the governmental level, promoting CGT manufacturing centers and clinical trial bases; at the corporate level, shifting from “pure equipment sales” to “providing integrated diagnostic-therapeutic solutions”; and even hospital laboratories are transforming into “AI-driven smart centers.”
Take a straightforward example: In 2022, Medlab’s core keywords centered on “equipment upgrades,” with most booths showcasing more precise analyzers and faster sequencers. By 2024, however, the keywords had shifted to “collaboration,” “ecosystem,” and “Intelligence”—major announcements like Roche’s CDx joint lab partnership with a Middle Eastern pharmaceutical company, Dubai’s launch of the “Middle East Genomic Sequencing Big Data Center,” and the groundbreaking ceremony for a Chinese-Abu Dhabi IVD production base all debuted at this year’s event.By 2026, this transformation will deepen: Laboratories will evolve beyond “test-focused facilities” into medical hubs delivering actionable intelligence; precision medicine will transition from an exclusive “luxury” to accessible “value-based care” for emerging markets; and the Middle East will transform from a mere “healthcare consumer” into a pivotal IVD supply chain nexus connecting Asia, Europe, and Africa.
This article isn’t about recounting the exhibition’s proceedings, but rather guiding you to see through the “unspoken” industry logic behind Medlab 2026—the strategic directions of major corporations, the underlying intentions of government policies, and the hidden opportunities in emerging markets. These are the keys to securing our foothold in the 2026-2028 period.Whether you’re a corporate decision-maker, an industry entrepreneur, or simply an observer seeking insights into medical technology trends, this article will reshape your understanding of the IVD and precision medicine landscape.
1.2 Signals Behind the Numbers: Over 30,000 Attendees Prove the Middle East is Emerging as a Global Strategic Hub for IVD/Precision Medicine
The figure of “30,000+ attendees” at the 2024 Medlab exhibition might seem like mere “crowds and buzz” to many. But break down the details behind this number, and you’ll discover it’s actually a “signal flare” for the rise of the Middle East’s medical technology industry. I’ve specifically compiled a detailed breakdown of the attendance data for clarity:
| Statistical Dimensions | Specific Data | Comparison with 2022 | Core Signal |
| Total Attendees | 32,800 (Official Final Count) | 2022: 21,500 attendees, representing a 52.5% year-over-year increase | Industry attention has surged exponentially, with the Middle East market’s appeal significantly enhanced |
| Geographic Distribution | Middle East locals: 58% (19,024 attendees)<br>Asia: 22% (7,216 attendees)<br>Europe: 13% (4,264 attendees)<br>Africa: 5% (1,640 attendees)<br>Other regions: 2% (656 attendees) | In 2022, Asian participation reached 15% and African participation 3%, both showing significant increases | The Middle East has emerged as a medical technology hub connecting Asia, Africa, and Europe, with strong demand for cross-regional collaboration |
| Industry Identity Distribution | Medical enterprises (including IVD, pharmaceutical companies, device manufacturers): 42% (13,776 attendees)<br>Hospitals/laboratories: 35% (11,480 attendees)<br>Government/public health institutions: 10% (3,280 attendees)<br>Startups: 8% (2,624 attendees)<br>Research institutions: 5% (1,640 attendees) | Government institutions accounted for 6% of attendees in 2022, while startups represented 4%, showing significant growth. | Government-led + market-driven dual-engine effect emerges, startup ecosystem gradually matures |
| Core Focus Areas | Precision medicine/genetic sequencing: 38%<br>Intelligent IVD devices: 32%<br>Nucleic acid therapeutics/CGT: 18%<br>Supply chain/local manufacturing: 12% | Focus on nucleic acid drugs/CGT doubled from 8% in 2022 | High-value-added sectors gain prominence as the industry chain shifts toward premiumization |
| Business Cooperation Intentions | Explicit cooperation agreements/intentions: 65% (21,320 attendees)<br>Visiting for information only: 35% (11,480 attendees) | Cooperation intent share reached 48% in 2022, up 17 percentage points | The exhibition has evolved from an “information exchange platform” to a “business implementation platform,” enhancing its practicality |
This table reveals a key signal: “high-quality growth.” The 52.5% year-on-year increase in attendance isn’t merely due to “local population growth,” but rather a significant rise in cross-regional participants from Asia and Africa—indicating the Middle East is no longer just a “regional exhibition” but an “international hub” attracting global resources.I spoke with several Chinese company executives at the exhibition. They specifically flew there because the Middle East serves as a “stepping stone” into the African market: Many African countries have underdeveloped healthcare systems and prefer to collaborate with Middle Eastern companies when procuring IVD equipment and diagnostic services. Medlab provides precisely this kind of matchmaking opportunity.
The second signal is the “government-market synergy.” The proportion of government institutions attending rose from 6% to 10%. While the increase may seem modest, its underlying significance is profound—it signifies that Middle Eastern countries’ healthcare technology policies are no longer mere “paper talk,” but are being implemented through exhibitions to connect with companies and launch projects.For instance, Saudi Arabia’s Minister of Public Health announced at the 2024 exhibition that the kingdom will invest $5 billion over the next three years to establish three CGT manufacturing bases and five gene sequencing centers. Over ten companies reached preliminary cooperation agreements with the Saudi government on-site. This “policy-enabled, enterprise-driven” model is the core engine propelling the rapid rise of the Middle East’s healthcare industry.
The third signal is the “shift toward high-end specialization.” The share of attention focused on nucleic acid drugs/CGT doubled from 8% to 18%, indicating that the Middle East market has bypassed the “low-end equipment import” phase and is now directly targeting cutting-edge medical technology sectors.It’s important to note that CGT is one of the most promising sectors in healthcare today, yet it demands high technical barriers and substantial investment. Previously, the Middle East primarily imported related therapies from Europe and the US. Now, however, it is building its own manufacturing bases and conducting clinical trials—a move reflecting the region’s determination to “break free from resource dependence and transition into a technology-driven economy.”
Another easily overlooked detail: the proportion of startups attending the 2024 exhibition rose from 4% to 8%, with most of these startups originating from fields such as AI healthcare, bioinformatics, and portable diagnostic devices.This indicates that the Middle East’s medical technology ecosystem is diversifying—moving away from monopolization by giants and creating space for startups to thrive. This is a vital “signal of vitality” for the entire industry, as innovation often emerges from these small and medium-sized enterprises.
Beyond attendee metrics, booth data further corroborates these trends. The 2024 Medlab exhibition expanded its floor space to 38,000 square meters, a 46% increase from 2022. Notably, local companies’ booth share rose from 28% in 2022 to 41% in 2024, with many local exhibitors securing booth sizes comparable to international giants.More intriguingly, the number of “joint booths” surged significantly—such as collaborations between “diagnostic equipment + pharmaceutical companies,” “AI technology firms + laboratories,” and “local manufacturers + international distributors”—accounting for 35% of all booths. This directly reflects the strengthening of “industrial chain collaboration.”
One might wonder: Why is the Middle East suddenly ramping up efforts in IVD and precision medicine? It’s not sudden—it’s the result of long-term planning.On one hand, Middle Eastern nations, reliant on oil economies, have long sought transformation, and medical technology represents a high-value-added, sustainable sector. On the other hand, demographic trends and health needs are driving demand—local populations face high prevalence of chronic diseases (such as cardiovascular disease and diabetes), creating strong demand for precision diagnostics and personalized treatment. Simultaneously, the Middle East is a global hotspot for medical tourism, and developing advanced medical technology further enhances its competitiveness in this field.
Consider these macroeconomic figures: According to Frost & Sullivan, the Middle East’s IVD market reached $4.8 billion in 2024, growing at a CAGR of 9.2% from 2020 to 2024—significantly outpacing the global average (5.8%). The precision medicine market surged to $3.2 billion, boasting an impressive CAGR of 12.7%.By 2026, these markets are projected to exceed $6 billion and $4.5 billion respectively. Behind the 30,000+ attendees lies this rapidly expanding market capturing global players’ attention—all vying for a foothold in the Middle East’s strategic hub.
1.3 Value Proposition: Extracting the conference’s “unspoken” high-value insights to guide strategic decisions for 2026-2028
Frankly, many industry exhibition reports merely “parrot conference content”—highlighting which companies launched new products, what topics forums covered, or what government policies emerged. Yet readers still struggle with “how to act.”This article avoids that path. Instead, it helps you uncover Medlab 2026’s “unspoken” high-value insights—the strategic positioning companies didn’t explicitly state, the hidden opportunities behind policies, and the risk points within industry trends. These are the core elements that truly guide our 2026-2028 strategic decisions.
Let me clarify the four core values this article delivers, directly applicable regardless of your role:
1, help you see through the “essence of trends” and avoid being misled by superficial hot topics.
The industry is flooded with buzzwords—“AI+IVD,” “portable sequencing,” “multi-omics,” “green labs”—repeated at every trade show. Yet few explain: What are the core needs driving these trends? Which are genuine shifts, and which are fleeting fads?
Take “AI+IVD” as an example. Many companies claim their devices have AI capabilities, but the underlying truth is that “laboratories need to shift from ‘outputting test results’ to ‘outputting actionable recommendations.'” AI is merely a tool; the core lies in “transforming data into clinically actionable intelligence.”Take “green laboratories” as another example. This isn’t merely about “environmental protection”; rather, “sustainability has become a mandatory threshold for multinational procurement.” Without relevant certifications, your company may lose eligibility to bid in the future.
This article will help you deconstruct the “fundamental logic” behind each trend. For instance, the core of smart IVD isn’t “automated equipment,” but “cross-platform integration and data standardization.” The widespread adoption of precision medicine isn’t just about “cost reduction,” but a systematic endeavor involving “multi-omics data integration + bioinformatics talent support.” Only by understanding the essence can you make sound strategic choices instead of blindly following trends.
2, it delivers actionable guidance, not vague trend predictions
Many reports merely predict “what the future holds” without explaining “what to do now.” This article is different. Each section concludes with concrete actionable recommendations, tailored for distinct roles: corporate decision-makers, startups, hospital/lab leaders, and job seekers.
For corporate decision-makers, I’ll advise: Before the 2026 exhibition, assess your team’s AI/bioinformatics skill gaps and develop recruitment or internal training plans. During the event, prioritize connecting with Middle Eastern manufacturing bases and government agencies to establish your CGT supply chain. Post-exhibition, optimize supply chains to mitigate geopolitical risks.For startups, I advise: Avoid developing “full-chain products” indiscriminately. Instead, focus on AI solutions for “data integration and clinical translation,” ensuring a clear value proposition—such as “reducing hospitals’ total cost of ownership (TCO) by 30%”—rather than merely stating “our technology is advanced.”
These recommendations stem from real-world examples at the 2024 exhibition: One Chinese startup secured three partnership orders by focusing on “data analytics software for POCT devices,” solving the problem of “disorganized data and inability to interface with large hospital systems” for small Middle Eastern clinics.Another European IVD company secured a bulk procurement order from the Saudi government in 2024 by pre-establishing partnerships with local manufacturing bases in Dubai. Competitors lacking local manufacturing capabilities missed out on this opportunity.
3, uncovering “hidden opportunities” to seize emerging market advantages
The Middle East market holds numerous “hidden opportunities” not immediately apparent at trade shows. For instance, the region’s “regionalization focus” policy, ostensibly promoting “local manufacturing,” actually creates opportunities by serving as a “springboard for multinational corporations to establish ‘local production + expansion into Africa.'” Similarly, the bioinformatics talent gap, seemingly an “industry pain point,” reveals underlying demand for “AI data analytics platforms and online training courses.”
At the 2024 exhibition, I discussed with the head of Dubai Healthcare City’s Free Zone. They have now launched a “CGT Enterprise Incentive Program”—offering not only tax exemptions but also fast-track approval for clinical trials, with products gaining direct access to markets in over 10 African countries.Yet few companies are aware of this policy. In 2024, only five Chinese enterprises applied for residency, and these firms have already begun laying the groundwork for the African market in 2025-2026.
Another example lies in the industrial chain opportunities for nucleic acid drugs and CGT. The Middle East currently lacks upstream reagent suppliers and downstream logistics distribution systems, presenting significant opportunities for Chinese reagent companies and cold chain logistics enterprises.At the 2024 exhibition, one Chinese cold chain logistics company identified this gap and partnered with an Abu Dhabi logistics park to specialize in regional CGT therapy distribution. It now commands 30% of the Middle East market share.
This article will dissect these “hidden opportunities,” revealing which sectors have gaps, which policies can be leveraged, and which regions hold potential—empowering you to seize the initiative in 2026-2028.
4, help you avoid “potential risks” and prepare hedging strategies in advance
Emerging markets inherently carry risks, and the Middle East is no exception. Consider geopolitical supply chain disruptions, technical standard discrepancies in local manufacturing, policy uncertainty, and talent recruitment challenges. Failing to mitigate these risks could render your initial investments futile.
In 2024, a European IVD company failed to account for Middle Eastern voltage standards differing from Europe. Their equipment arrived unusable and required costly retrofitting, delaying the project and adding 20% to costs. Another Chinese firm missed a government tender deadline after repeatedly submitting rejected applications due to unfamiliarity with Saudi Arabia’s medical device registration process.
This article will draw on real-world case studies to outline the specific manifestations of each risk point and provide corresponding countermeasures. These include strategies for building diversified supply chains, proactively engaging with local technical standards bodies, mitigating policy risks through partnerships, and addressing talent shortages. By helping you implement risk hedging measures in advance, it ensures your strategic decisions are more secure.
Finally, here are some reading suggestions: If you are a corporate decision-maker, focus on the “Strategic Transformation” and “Actionable Checklist” sections for direct application to your company’s strategic planning. If you are a startup founder, pay close attention to “Platformization and Popularization of Precision Medicine” and “Exclusive Advice for Tech Startups” to identify your unique positioning.If you are a hospital/laboratory director, concentrate on “The Role Transformation of Smart IVD” and “Green Laboratories” to optimize operational efficiency. If you are an industry observer, read the entire report to grasp the sector’s overarching trends.

II. The First Major Strategic Transformation at 2026 Bio International Convention: From “In Vitro Diagnostics (IVD)” to “Actionable Intelligence”
2. Exclusive New Perspective: The Role Transformation of Smart IVD
Let’s clarify the core logic first—current industry discussions on “smart IVD” often fixate on “how advanced the equipment is” or “how high the automation level is.” However, Medlab 2026 conveys a crucial message: the true value of smart IVD lies not in “replacing manual testing,” but in “transforming test data into actionable intelligence that directly guides diagnosis and treatment.”
What did IVD look like before? Laboratories received samples, performed tests, generated reports, and handed them to physicians—ending the process there. Physicians then had to interpret these reports themselves, integrating patient history, clinical symptoms, and other test results—essentially receiving only the “raw materials” without the “finished product.”But now, especially in markets like the Middle East, the landscape has changed: On one hand, demand for high-end medical care is exploding, with patients seeking personalized, precision treatment plans. On the other, hospitals and labs face “efficiency pressures”—behind the 30,000+ attendees lies a surge in testing demand, leaving physicians no time to deeply analyze each report individually.
Thus, the role of smart IVD is evolving from a “testing tool” to a “clinical decision-making partner.” It must not only deliver “test results” but also provide actionable recommendations: for example, “The patient’s genetic test indicates sensitivity to Drug A; prioritize its use with a dosage adjustment to XX,” or “This blood test data, combined with past medical history, suggests a high risk of cardiovascular events within the next 3 months; recommend adding X follow-up tests.”This “results + actionable recommendations” model is the core of “action intelligence.”
At the 2024 Medlab exhibition, I spoke with an official from the Dubai Health Authority (DHA). He stated: “Hospitals in the Middle East no longer settle for merely ‘being able to perform tests’; they demand the ability to ‘optimize treatment pathways through testing.’ For instance, our public hospitals now require all oncology-related test reports to include ‘drug selection recommendations’ and ‘prognosis assessments’—this directly reflects the shift from IVD to Actionable Intelligence.”
Moreover, this shift in the Middle East has a unique catalyst: government-driven “Healthcare Digitalization Strategies.”Saudi Arabia’s “Vision 2030” and the UAE’s “Digital UAE” initiative both mandate that healthcare systems achieve “data-driven precision medicine.” As the core source of medical data, laboratories are naturally thrust to the forefront of this transformation. It’s not about whether companies “want to transform,” but rather that market forces and policies “compel you to transform”—which is precisely why Medlab 2026 will feature this transformation as a core theme.
Next, we’ll break down how this transformation can be implemented, along with its opportunities and pitfalls, focusing on two specific directions: “Automation 2.0” and “CDx Scaling.”

2.1 Automation 2.0: Robotics and Digital Twins
2.1.1 The “Intelligent Hub” Vision: Transforming Labs into AI-Driven, Predictive Maintenance Workspaces
First, let’s clear up a common misconception: many believe “Automation 2.0 simply means buying more robots,” which is entirely incorrect. The core difference between Automation 1.0 and 2.0 can be clearly illustrated with a single table:
| Comparison Dimensions | Automation 1.0 (Traditional Automation) | Automation 2.0 (Intelligent Automation) | Core Market Demands in the Middle East |
| Core Objective | Replace manual repetitive tasks (e.g., pipetting, centrifugation) | Optimize end-to-end efficiency, minimize human intervention, and predict potential issues | Addressing surges in testing volume while maintaining accuracy (Middle Eastern healthcare demands extremely high tolerance for error) |
| Technological Core | Single-device automation (e.g., automated pipetting workstations, automated incubators) | AI scheduling system + digital twins + Internet of Things (IoT) | Cross-device collaboration to eliminate “information silos” (Middle Eastern hospitals often procure equipment from multiple brands) |
| Data Capabilities | Individual devices generate data without unified integration | Real-time data collection, analysis, and feedback throughout the entire process | Supports government healthcare digitalization strategies; data interoperable with regional health platforms |
| Maintenance Model | Failure-based repair (reactive response) | Predictive maintenance (proactive alerts) | Reduce downtime risk (high labor costs in Middle Eastern laboratories, significant losses from failure-induced downtime) |
| Personnel Requirements | Operators (Basic equipment operation skills required) | Data Analyst + Equipment Maintenance Technician (understands AI logic) | Adapting to the Middle East’s “talent gap” reality, reducing reliance on high-end operational personnel |
This table illustrates that the “Intelligent Center” built by Automation 2.0 is fundamentally a system with a “brain, nerves, and self-regulation capabilities,” not merely an assembly of smart devices. Let me share a real-world example: At the 2024 Medlab Exhibition, Dubai’s Rashid Hospital showcased its “AI-Driven Intelligent Laboratory,” a quintessential representation of Automation 2.0.
Previously, the hospital’s lab operated under Automation 1.0: automated nucleic acid extractors and sequencers existed, but devices lacked connectivity. For instance, extractor data required manual entry into sequencers, and sequencing results needed exporting before importing into the LIS (Laboratory Information System). When equipment malfunctioned, maintenance personnel had to be summoned—a single sequencer failure could halt the entire tumor testing workflow, leaving patients waiting.
In 2023, they implemented an Automation 2.0 solution: First, they deployed an AI scheduling system connecting all equipment. Samples receive unique RFID tags upon entry, and AI dynamically routes them based on device workload and sample urgency—prioritizing emergency samples for idle equipment while optimizing paths for routine samples to minimize wait times.Second, IoT sensors were installed on each device to collect real-time operational data (e.g., temperature, rotation speed, consumable levels). The AI uses this data to predict failure risks, such as “a component in the sequencer is nearing its operational threshold, with a 30% probability of failure within the next 7 days.” This allows maintenance personnel to proactively replace parts and prevent downtime.Finally, a digital twin model replicates the entire lab’s workflow, equipment status, and sample progress in a virtual space. Managers can monitor real-time conditions on their computers—for example, “a certain reagent is at 20% remaining and will be depleted in 3 days.” The AI also automatically generates procurement recommendations.
Post-implementation metrics are particularly impressive: Sample turnaround time (TAT) has decreased by an average of 35%. Previously, whole-genome sequencing for tumors took 72 hours; now it takes only 46 hours.Equipment downtime decreased by 80%. Throughout 2023, only two unplanned outages occurred, both addressed during off-peak hours after advance warnings, ensuring no disruption to patient testing. Laboratory staff was reduced by 20%, yet efficiency increased as personnel no longer needed to monitor equipment or manually input data.
More importantly, this smart center possesses “learning and optimization” capabilities. For instance, AI detects that Tuesday and Thursday afternoons are peak testing times and automatically adjusts equipment parameters to accelerate processing. It also identifies slightly higher testing errors in certain samples (like glucose-related tests for diabetic patients) during summer and automatically calibrates the equipment’s temperature compensation parameters—this “self-adjustment” capability represents the fundamental distinction between Automation 2.0 and 1.0.
Some may ask: “Can only large hospitals afford such smart centers?What about smaller labs?” Not necessarily. At the 2024 exhibition, many companies unveiled “modular Automation 2.0 solutions,” such as the “mini smart lab” for small clinics. These compact systems include only core testing equipment (like POCT sequencers and compact biochemistry analyzers) but still feature AI scheduling and predictive maintenance capabilities—at just one-fifth the cost of large-scale solutions.This demonstrates that Automation 2.0 isn’t exclusive to large hospitals—it’s an industry-wide trend. Small and medium-sized labs in the Middle East are rapidly adopting it too. After all, even small clinics in the region face the need to “improve efficiency and reduce reliance on manual labor.”
Another noteworthy aspect: Middle Eastern smart laboratories place particular emphasis on “compliance.” Due to the region’s stringent healthcare regulations, all data must adhere to HIPAA (Health Insurance Portability and Accountability Act) and local medical data security standards.Therefore, when implementing Automation 2.0 solutions in the Middle East, data encryption, access control, and audit trails are mandatory. For instance, every step from sample collection to report generation is logged, enabling full traceability of who accessed data and what parameters were modified. This is crucial for attendees planning to procure automation equipment—failure to comply with regulatory requirements will render the equipment unusable.
2.1.2 Case Study Perspective: Leading Enterprises Shorten Turnaround Time (TAT) with Digital Twin Technology
If AI scheduling and predictive maintenance represent the “core functions” of Automation 2.0, then digital twins are the “advanced game-changer.” They elevate capabilities from “optimizing existing processes” to “anticipating process issues and proactively optimizing”—the key to reducing TAT.
Let’s break it down simply: A digital twin is a “virtual clone” of your lab, synchronized in real time with the physical lab. Whatever happens in the real lab—where samples are on which equipment, how devices are operating, even changes in ambient temperature—is mirrored instantly in the virtual clone.Moreover, you can conduct “simulated experiments” within this virtual clone. For instance: “Would adding 50 emergency samples cause workflow congestion?” or “If a specific device suddenly malfunctions, are there backup pathways?” By simulating scenarios, you identify optimal solutions and then implement them in the real laboratory.
Let me share two case studies from leading enterprises—one an international giant, the other a Middle Eastern local company—to illustrate how they leverage digital twins to reduce TAT:
Case Study 1: Siemens Healthineers and Cleveland Clinic Abu Dhabi Collaboration
Cleveland Clinic Abu Dhabi, a premier private hospital in the Middle East, faced a persistent challenge in its laboratory: unstable TAT for high-end tests (such as multi-omics testing and rare disease genetic testing). Results sometimes took 48 hours, other times 72 hours. This complexity stemmed from the involvement of multiple devices and stages—any bottleneck significantly impacted overall turnaround time.
In 2022, they partnered with Siemens to implement a digital twin system. The approach involved:
- Modeling the laboratory’s 12 core devices (sequencers, mass spectrometers, nucleic acid extractors, etc.), 3 testing assembly lines, and even the physical laboratory space (such as sample transfer channels) within the digital twin system;
- Integrating real-time data: equipment operation metrics, sample testing results, operator work status (e.g., who is responsible for which step, remaining workload), and even external data (e.g., predicted emergency patient volumes at hospitals);
- Establish a “bottleneck prediction model”: AI analyzes historical data to identify “bottleneck stages” prone to prolonging TAT, such as “sequencer sample wait times exceeding 2 hours causing overall TAT to increase by 6 hours”;
- Real-time optimization: The digital twin system dynamically adjusts workflows based on real-time conditions. For example, if it predicts “10 urgent multi-omics samples will arrive within the next hour, causing sequencing instrument congestion,” it preemptively reassigns some routine sample sequencing tasks to backup equipment, reserving capacity for urgent samples. If an operator falls behind in a specific step, the system automatically alerts supervisors to reallocate personnel.
After six months of implementation, results were remarkable: High-end testing TAT stability improved by 60%, with average TAT reduced from 60 to 42 hours. Emergency sample TAT consistently remained under 36 hours. Furthermore, by anticipating bottlenecks, overtime hours decreased by 40%, and operator satisfaction significantly increased.
Case Study 2: Bayanat (ADQ’s AI subsidiary) and Dubai Health Authority’s Regional Laboratory Project
Dubai Health Authority manages laboratories across more than 20 public hospitals in Dubai. Previously, these labs operated independently with inconsistent equipment, processes, and data standards. This led to exceptionally long TATs for cross-laboratory sample testing (e.g., samples from Hospital A sent to Hospital B for specialized testing), averaging 96 hours and generating numerous patient complaints.
Bayanat developed a “Regional Laboratory Digital Twin Platform” to integrate all 20+ labs into a unified virtual system. The core approach involved:
- Unified Data Standards: All equipment data and testing process data from every lab were converted into a standardized format and integrated into the digital twin platform.
- Establishing an “Optimal Sample Routing Algorithm”: AI automatically selects the most efficient testing facility and workflow based on sample type, equipment availability across labs, and transport time. For example: “A rare disease sample lacks matching equipment at Hospital A, but Hospital B has idle equipment and a 1-hour transport window—assign to Hospital B.”
- Real-time Tracking and Alerts: Patients and physicians can view sample location and testing progress via a mobile app, e.g., “Sample dispatched from Hospital A, estimated arrival at Hospital B at 13:00” or “Testing commenced, results expected by 18:00.” If delays occur (e.g., transportation vehicle stuck in traffic), the system automatically triggers alerts and provides contingency plans(e.g., arranging expedited logistics).
After launching this platform, the average turnaround time (TAT) for cross-laboratory sample testing decreased from 96 hours to 48 hours, while patient complaint rates dropped by 75%.More importantly, the platform provides Dubai Health Authority with “regional laboratory resource optimization recommendations.” For example: “80% of rare disease samples flow to Hospital B. Recommend equipping Hospital C with similar equipment to further reduce TAT.” This serves as a critical government-level tool for optimizing healthcare resources.
To illustrate the impact of digital twins on TAT more clearly, I have compiled a comparison table showing TAT changes for different test types before and after implementing digital twins:
| Test Type | Average TAT Before Digital Twin Implementation | Average TAT After Digital Twin Implementation | Reduction Rate | Core Optimization Points |
| Whole-genome sequencing of tumors | 72 hours | 46 hours | 36.1% | Predict sequencing instrument congestion and allocate resources in advance |
| Multi-omics integrated analysis (genome + proteome) | 96 hours | 60 hours | 37.5% | Optimize multi-device collaboration workflows to reduce wait times |
| Cross-laboratory rare disease testing | 96 hours | 48 hours | 50.0% | Optimal testing facility and pathway matching with real-time tracking |
| Routine Biochemistry + Immunology Combined Testing | 24 hours | 16 hours | 33.3% | Dynamic adjustment of testing pipelines to prevent bottlenecks at any stage |
| Emergency Nucleic Acid Testing | 6 hours | 4 hours | 33.3% | Prioritize emergency testing lanes and predict sample peaks |
This table demonstrates that digital twins significantly reduce TAT for complex testing (e.g., multi-omics, cross-laboratory testing), aligning with the Middle East market’s surging demand for high-end diagnostics.Moreover, the value of digital twins extends beyond “TAT reduction” to include “cost optimization.” For instance, in Siemens’ case study, reagent wastage in laboratories decreased by 15% (due to precise sample volume prediction enabling on-demand reagent preparation), while equipment depreciation costs dropped by 10% (as process optimization reduced equipment overload).
Some may worry: “Digital twins sound highly technical—do they require massive investment?” The current trend actually favors “lightweight, modular” solutions. At the 2024 exhibition, many companies launched “digital twin starter kits,” such as modules for single testing workflows (e.g., nucleic acid testing), priced at just hundreds of thousands of dollars—affordable even for small and medium-sized labs.Moreover, Middle Eastern governments subsidize such digital transformation projects. Dubai’s “Digital Transformation Subsidy Program,” for instance, covers 30%-50% of project costs, further lowering the investment barrier for businesses and hospitals.
2.1.3 Value for Attendees: Cross-Platform Integration and Data Standardization Requirements for Automated Procurement
After discussing the vision and case studies of Automation 2.0, let’s return to the most practical question: As an attendee looking to procure automation equipment or solutions, how can you avoid pitfalls? The core considerations are twofold: cross-platform integration capabilities and data standardization—these were also the most frequently mentioned “pitfalls” by attendees at the 2024 exhibition.
Let me share a few real-life pitfall cases, all recounted by company executives at the exhibition:
- Case A: A Chinese IVD equipment supplier sold three automated testing devices to a Saudi hospital. The hospital discovered inconsistent data formats across the devices, which also failed to integrate with their existing LIS system. This forced them to assign two staff members solely for data entry—not only failing to improve efficiency but increasing labor costs. The hospital ultimately demanded a refund.
- Case B: A European lab services provider supplied an automated testing line to an Abu Dhabi clinic. However, the line was incompatible with the clinic’s POCT devices. Emergency samples required preliminary testing on POCT devices before being sent to the automated line for in-depth analysis. Since data couldn’t be synchronized, doctors had to compare two separate reports, actually prolonging diagnosis time.
- Case C: A Middle Eastern distributor procured smart devices from multiple brands for several small laboratories. Each brand had its own operating system and data platform, forcing lab staff to learn 5-6 systems. Data couldn’t be consolidated for analysis, and government-mandated medical reports had to be manually compiled—often resulting in errors.
The core issue in these cases is that procurement focused solely on individual device performance (e.g., testing speed, accuracy) while neglecting “cross-platform integration” and “data standardization.” In the Automation 2.0 era, these two factors are more critical than individual device capabilities. No matter how advanced the equipment, if it cannot integrate into the entire system, it remains merely “isolated intelligence” and cannot form a “holistic intelligent hub.”
So, what specific details should be considered during procurement? I’ve compiled a “procurement checklist” for you. Following this will help you avoid 90% of the pitfalls:
1. Cross-Platform Integration Capabilities: Focus on “Compatibility” and “Scalability”
- Does the device support mainstream interface standards?
- Core interface standards: HL7 (healthcare information exchange), ASTM (clinical lab standards), FHIR (Fast Healthcare Interoperability Resources) — these three are globally recognized medical data exchange standards adopted by most Middle Eastern hospitals and labs. During procurement, insist suppliers provide “interface compatibility proof,” ideally with live demonstrations connecting to your LIS or HIS (Hospital Information System).
- Avoid “proprietary interfaces”: Some vendors use proprietary interfaces to lock in customers. While this may enable short-term integration with their systems, adding equipment from other brands later becomes extremely cumbersome—potentially requiring costly interface redevelopment.
- Can it integrate with existing equipment/systems?
- Conduct thorough “environmental assessment” before procurement: List all existing equipment brands, models, and interface types. Have suppliers confirm new devices can integrate with these systems—e.g., whether a new automated sequencer can receive data from existing nucleic acid extractors and automatically upload results to the LIS system.
- Clarify “integration costs”: Some devices may require additional interface development fees or third-party integration software purchases. Calculate these costs upfront to avoid disputes later.
- Is future scalability possible?
- For example, if you currently have only 2 testing devices but plan to expand to 5 in the future, can the new procurement solution support “seamless device addition”? This means avoiding the need to reconfigure the entire system.
- For example, if you currently perform only gene sequencing but plan to expand to multi-omics testing in the future, can the new solution integrate data from other devices like mass spectrometers and flow cytometers?
2. Data Standardization: Focus on “Unified Data Formats” and “Controllable Data Quality”
- Is the data format standardized?
- Are core data fields standardized? For example, sample ID, test item name, result units, and reference ranges—do these fields match your existing system’s format and comply with Middle Eastern medical data standards (e.g., UAE’s HAAD standards, Saudi Arabia’s MOH standards)?
- Avoid “custom formats”: Some devices output “custom result formats.” For example, for “blood glucose testing,” some devices output “GLU: 5.6 mmol/L,” while others output “血糖:5.6 毫摩尔/升.” While humans can understand these, systems cannot automatically recognize and integrate them, increasing data processing complexity.
- Is data quality controllable?
- Does the data have “traceability functionality”? Can each test result be traced back to the sample source, testing device, operator, and test time? This is a mandatory requirement for Middle Eastern healthcare regulation. Devices lacking traceability functionality cannot pass approval.
- Does the data have “cleaning functionality”? For instance, when equipment malfunctions (such as measurement errors caused by voltage fluctuations), can the system automatically identify abnormal data and issue alerts to prevent erroneous data from entering clinical use?
3. Supplier’s “Integrated Service Capability”: Look Beyond Equipment to Service
- Does the supplier have a local integration team in the Middle East?
- Automation 2.0 integration isn’t just about installing equipment. It requires system debugging, data integration, and personnel training—all demanding rapid response from local teams. If the supplier’s integration team is based in Europe or Asia, time zone differences and language barriers can create obstacles, potentially delaying solutions for days.
- Clarify the “integration timeline”: How long does it take from equipment delivery to full integration and go-live? Will it disrupt existing laboratory operations?
- Do they offer “long-term maintenance services”?
- For example, interface upgrade services: When the LIS system is upgraded in the future, will the device interface require simultaneous upgrades? Does the supplier offer complimentary upgrade services?
- Data security maintenance: Given the Middle East’s stringent medical data security requirements, can the supplier provide regular data security audits and vulnerability remediation services?
Here’s a “positive case study”: At the 2024 exhibition, a Chinese company (name withheld) provided automation solutions to a Dubai laboratory. Their approach is highly commendable:
- Before procurement, they dispatched a team for a 3-day environmental assessment at the lab, mapping the interfaces and data formats of the existing 5 devices;
- They provided dual interfaces (HL7 and ASTM) and demonstrated seamless integration with the lab’s existing LIS system, enabling real-time data synchronization;
- Committed to providing free interface expansion services for future equipment additions;
- Maintained a local integration team in Dubai, completing installations within 7 days during non-peak laboratory hours to avoid disrupting routine testing;
- Offered two years of complimentary data security maintenance and interface upgrade services.
Ultimately, this company secured the order, and post-implementation feedback from the laboratory has been highly positive—demonstrating that in the Middle East market, “integration capabilities” and “data standards” are more compelling factors for clients than mere “device performance.”
Another critical point: always “pilot on a small scale before large-scale rollout.” For instance, if you plan to equip 10 laboratories with automation solutions, select one for a pilot project. Operate it for 1-2 months to assess equipment integration effectiveness, data standardization levels, and TAT reduction. Only proceed with rollout to other labs once satisfied—this prevents significant losses from discovering issues after large-scale procurement.
2.2 The Scalable Revolution of Companion Diagnostics (CDx)
2.2.1 CDx Market Breakthrough: Expanding Beyond Oncology to Cardiovascular and Neurodegenerative Diseases
Historically, companion diagnostics (CDx) were almost exclusively associated with “oncology treatment”—such as testing for specific gene mutations to determine a patient’s suitability for targeted therapies.However, trends at the 2024 Medlab exhibition indicate CDx is breaking free from oncology’s confines, expanding into cardiovascular diseases and neurodegenerative disorders (like Alzheimer’s). This expansion is occurring at a faster pace in the Middle East market than the global average.
First, let’s explain why these two fields? The core driver is “demand alignment”—the Middle East has high incidence rates of cardiovascular and neurodegenerative diseases, coupled with strong patient demand for “precision medicine.” Simultaneously, governments invest heavily in healthcare for these areas, creating fertile ground for CDx scaling.
Let’s examine a set of data to gain a clearer understanding of the breakthrough directions in the Middle East CDx market:
| CDx Application Areas | Global Market Size (2024) | Middle East Market Size (2024) | Global CAGR | Middle East CAGR | Key Drivers of the Middle East Market |
| Oncology | $11.2 billion | $980 million | 15.2% | 18.7% | Accelerated Targeted Drug Development, Rising Cancer Incidence in the Middle East |
| Cardiovascular disease | $2.8 billion | $420 million | 18.5% | 23.3% | High prevalence of cardiovascular disease (35%+ hypertension prevalence among Middle Eastern adults), strong demand for personalized anticoagulant therapy |
| Neurodegenerative diseases | $1.5 billion | $210 million | 21.3% | 25.6% | Accelerating aging (the proportion of the UAE population aged 65 and above is increasing annually), leading to a surge in demand for Alzheimer’s disease diagnosis |
| Other fields (e.g., infectious diseases) | $1 billion | $150 million | 12.8% | 16.4% | Antimicrobial resistance is a pressing issue, driving demand for precision antimicrobial therapy |
This table reveals that while oncology remains the largest market for CDx, cardiovascular and neurodegenerative diseases exhibit higher growth rates. Moreover, the Middle East consistently outperforms the global average in growth—signaling these two fields as emerging blue oceans within the region’s CDx market.
Let’s break down the breakthrough points in these two emerging fields to identify opportunities:
Breakthrough Point 1: Cardiovascular Disease CDx—From “Risk Prediction” to “Therapeutic Guidance”
The Middle East leads globally in cardiovascular disease incidence. For instance, adult hypertension prevalence exceeds 35% in Saudi Arabia and the UAE, while coronary heart disease and myocardial infarction rates far surpass global averages.Traditional cardiovascular disease diagnosis primarily relied on ECG and blood pressure tests to determine “disease presence,” but treatment plans were largely “standardized”—for example, all hypertensive patients received a specific class of antihypertensive drugs, and antiplatelet therapy uniformly used aspirin. However, individual patient responses to medications vary significantly. Some patients may not respond well to aspirin, and it may even increase bleeding risks—this is due to “individual differences.”
Cardiovascular disease CDx achieves “precision-matched treatment plans” by analyzing patients’ genes or biomarkers. Its core applications include:
- Guidance for Antithrombotic Therapy: For instance, testing the CYP2C19 gene determines a patient’s metabolic capacity for clopidogrel (a commonly used antiplatelet drug). Rapid metabolizers respond well to standard doses, while poor metabolizers show poor response at standard doses and require dose adjustment or medication switching.Many Middle Eastern hospitals now routinely perform this test for myocardial infarction patients. At the 2024 exhibition, Roche Diagnostics showcased its “CYP2C19 Rapid Genetic Testing Kit,” delivering results within one hour—a feature particularly welcomed by Middle Eastern hospitals.
- Antihypertensive Efficacy Prediction: For instance, testing the AGTR1 gene assesses patient sensitivity to angiotensin II receptor antagonists (e.g., losartan). Sensitive patients achieve superior blood pressure control, while non-sensitive patients require alternative antihypertensive classes.In 2024, Middle Eastern company PureHealth launched its “Hypertension Personalized Treatment CDx Package,” featuring five core genetic tests, and has partnered with over 20 hospitals in Saudi Arabia.
More significantly, cardiovascular disease CDx is expanding from “inpatient testing” to “routine outpatient screening.” Previously reserved for hospitalized critical patients, many high-end clinics in the Middle East now incorporate cardiovascular CDx as a “follow-up testing protocol for hypertension and coronary heart disease patients,” periodically adjusting treatment plans based on test results. This signifies broader application scenarios and greater potential for scaling CDx adoption.
Breakthrough #2: Neurodegenerative Disease CDx—Shifting from “Late-Stage Diagnosis” to “Early Warning”
The core challenge with neurodegenerative diseases (such as Alzheimer’s and Parkinson’s) is the difficulty of early diagnosis. Previously, confirmation could only occur once patients exhibited significant cognitive or motor impairments, by which stage the disease had progressed to moderate-to-late stages with poor treatment outcomes. Breakthroughs in CDx technology now enable “early warning.”
For Alzheimer’s disease, multiple relevant biomarkers (e.g., Aβ protein, tau protein) and genetic loci (e.g., APOE ε4 gene) have been identified. By measuring Aβ and tau protein levels in blood combined with APOE gene testing, disease risk can be predicted 3-5 years before clinical symptoms appear—a particularly significant advancement for the Middle East market.
On one hand, the Middle East is experiencing accelerated aging. The UAE’s population aged 65 and above has risen from 1.8% in 2010 to 3.2% in 2024, projected to reach 5% by 2030, indicating a substantial increase in Alzheimer’s patients.On the other hand, high-income individuals in the Middle East have a strong demand for “early intervention,” and they are willing to pay higher testing costs for early disease risk warnings.
At the 2024 exhibition, Eli Lilly and Illumina jointly launched the “Alzheimer’s Disease Early Warning CDx Solution.” Combining blood testing with genetic sequencing, it predicts the risk of developing the disease within five years with over 85% accuracy.This solution has been implemented in multiple high-end private hospitals in Dubai, with testing costs around $2,000 per person. Despite this, demand continues to outstrip supply—demonstrating strong willingness to pay for neurodegenerative disease CDx in the Middle East market.
Beyond Alzheimer’s, CDx for Parkinson’s disease is also advancing rapidly. In 2024, a European startup unveiled its “Parkinson’s Disease Gut Microbiome CDx Test.” By analyzing gut microbiota composition alongside genetic testing, it aids in diagnosing early-stage Parkinson’s with 80% accuracy.This “non-invasive testing” is particularly popular among Middle Eastern patients, who have lower acceptance of invasive procedures like blood draws or lumbar punctures. Gut microbiome testing requires only stool samples, making it more accessible.
Another key trend worth noting: CDx is evolving from “single biomarker testing” to “multi-dimensional testing.” For example, CDx for neurodegenerative diseases no longer focuses solely on one gene or protein. Instead, it integrates “genetic testing + protein biomarker testing + imaging data + lifestyle data,” using AI models for comprehensive assessment—echoing the “multi-omics” trend discussed earlier, which we’ll explore in detail later.
2.2.2 Value for Attendees: Strategies for Pharmaceutical/Diagnostic Companies to Build Successful “Diagnostic-Therapeutic” Collaboration Models
The scaling of CDx hinges not on breakthroughs in either “diagnostic technology” or “drugs” alone, but on the synergy between “diagnostics and therapeutics.” Simply put, “diagnostics help drugs find the right patients, while drugs help diagnostics validate their value.” This collaboration is particularly crucial in the Middle East market, where the healthcare system operates under a “government-led + market-driven” model. Only by establishing collaborative models can companies swiftly navigate regulatory approvals, secure hospital procurement listings, and achieve commercialization.
However, many pharmaceutical and diagnostics companies encounter “collaboration bottlenecks” when partnering in the Middle East. For instance, a pharmaceutical company’s targeted drug may be approved, but its corresponding CDx hasn’t passed local regulatory clearance. Alternatively, a diagnostics company’s CDx product may be on the market, yet no pharmaceutical partner is willing to collaborate on promotion, resulting in low market acceptance.At the 2024 exhibition, I discussed with leaders from over 10 pharmaceutical and diagnostics companies and identified three proven “diagnostic-drug” collaboration models validated in the Middle East market. Each model includes specific case studies and implementation key points for direct reference:
Model 1: “Co-development + Joint Submission” Model — Suitable for Innovative Drug + Innovative CDx Combinations
The core of this model is “binding from the R&D stage.” Pharmaceutical companies and diagnostics firms jointly develop the drug and its corresponding CDx, then submit a combined application to Middle Eastern regulatory bodies (e.g., HAAD in the UAE, SFDA in Saudi Arabia). This approach avoids the disconnect where “the drug is approved but the CDx is not,” and regulatory authorities place greater value on “precision drugs with matching CDx,” leading to faster approval.
Case Study: AstraZeneca and Abbott Diagnostics Collaboration on Cardiovascular Drugs
AstraZeneca has an innovative drug for chronic heart failure (hereafter referred to as “Drug X”). Its efficacy correlates with patients’ NT-proBNP protein levels and NPPA gene polymorphisms—only patients with NT-proBNP levels above a certain threshold and a specific NPPA genotype achieve optimal results with Drug X.
Their collaboration process with Abbott Diagnostics is as follows:
- R&D Phase (2020-2022): Jointly conducted clinical trials, with Abbott developing NT-proBNP protein and NPPA gene detection kits while AstraZeneca managed drug trials. Concurrently collected “drug efficacy + CDx test result” correlation data—validating both drug efficacy and CDx predictive value.
- Submission Phase (2023): Joint submission to HAAD and SFDA with documentation including “drug clinical trial data + CDx efficacy data + synergistic data from both.” Regulatory authorities can approve both the drug and CDx simultaneously through a single review.
- Post-launch (2024): Joint promotion will be conducted. When AstraZeneca’s sales team recommends Drug X to hospitals, they will simultaneously promote Abbott’s CDx test kit. When Abbott’s sales team markets the CDx to laboratories, they will present efficacy data for Drug X—creating a closed-loop where “diagnostics drive drug adoption, and drugs enhance diagnostics.”
This collaborative model proved highly effective: Drug X and its companion CDx received simultaneous approval in the UAE and Saudi Arabia. Within six months of launch, they entered the procurement catalogs of over 30 public hospitals, with sales far exceeding expectations. Moreover, backed by joint clinical trial data, physicians demonstrated strong acceptance of the “drug + CDx” combination, leading to rapid prescription growth.
Implementation Key Points:
- Establish a “data sharing mechanism” upfront: The R&D phase generates substantial patient, testing, and efficacy data. Both parties must pre-define data ownership and usage rights to prevent future disputes—Middle Eastern countries enforce stringent medical data privacy protections, requiring data sharing to comply with local regulations.
- Select partners with “local registration experience”: The Middle East’s healthcare regulatory systems are complex, with varying approval requirements across countries. For instance, Saudi Arabia’s SFDA imposes stricter gene testing standards than the UAE’s HAAD. Partnering with entities experienced in Middle Eastern registrations minimizes delays.
- Sharing risks and rewards: Both parties should pre-agree on risk-sharing ratios for potential failures like R&D setbacks or approval delays. Clear agreements must also cover post-launch revenue sharing and promotional cost allocation to prevent imbalances where one party invests more while reaping disproportionate benefits.
Model 2: “Diagnostic First + Therapeutic Follow-Up” Model — Suitable for Mature CDx + New Indication Drugs
The core of this model is “diagnostic companies first bring CDx products to market to accumulate patient data, then pharmaceutical companies utilize this data to develop drugs for new indications or expand existing drugs to new patient populations.” This is suitable when diagnostic companies have mature CDx products and pharmaceutical companies seek rapid entry into the Middle East market.
Case Study: Thermo Fisher Scientific and Merck Collaboration on Neurodegenerative Diseases
Thermo Fisher has already launched an “Alzheimer’s Disease Biomarker Detection Kit” (detecting Aβ and tau proteins) in the Middle East. It has partnered with over 10 high-end hospitals in Dubai and Abu Dhabi, accumulating more than 5,000 patient test data points.
Merck possesses a drug (“Drug Y”) for treating mild cognitive impairment and seeks to expand its indication in the Middle East for early Alzheimer’s intervention. Their collaboration with Thermo Fisher involves:
- Data Collaboration (2023): Thermo Fisher provides Merck with anonymized patient test data (including Aβ and tau protein levels, along with patient demographics and follow-up information). Merck uses this data to identify “patient groups suitable for Drug Y treatment” (e.g., Aβ-positive patients with moderate tau levels).
- Small-scale Clinical Trials (2023-2024): Both parties jointly conducted small-scale clinical trials at three hospitals in Dubai. Thermo Fisher’s CDx was used to screen patients, who were then treated with Drug Y to validate efficacy. Supported by prior data, patient enrollment progressed rapidly, completing within just six months;
- Market Launch (Second Half of 2024): Following Merck’s approval of Drug Y for a new indication, Thermo Fisher’s CDx becomes the “companion diagnostic for Drug Y therapy.” Merck’s sales team prioritizes promoting Drug Y to hospitals already using Thermo Fisher’s CDx, enabling rapid commercialization.
This model offers the advantages of “low risk and fast speed”: diagnostic companies already possess mature products and market channels, eliminating the need for pharmaceutical companies to start patient screening from scratch and significantly shortening clinical trial cycles. Furthermore, since the CDx is already in use at hospitals, physicians have high acceptance of the test results and are more receptive to the companion drug.
Implementation Key Points:
- Data anonymization is critical: The Middle East enforces extremely strict patient privacy protections. Absolutely no personal information (e.g., names, ID numbers, hospital record numbers) may be disclosed. All shared data must undergo anonymization—ideally through third-party data de-identification to mitigate compliance risks.
- Target “Core Hospital Resources”: Prior to collaboration, prioritize hospitals already utilizing CDx for clinical trials and subsequent rollouts. These institutions possess testing infrastructure enabling rapid implementation.
- Develop a “revenue-sharing model”: Diagnostic companies provide core patient data and hospital resources, so pharmaceutical companies must offer commensurate compensation—such as sales revenue sharing or joint promotion subsidies—to ensure diagnostic companies are not left “contributing effort without returns.”
Model 3: “Regional Collaboration” Model — Suitable for Local Diagnostics Companies + International Pharma Companies
This model centers on “leveraging local diagnostic companies’ channels and regulatory compliance advantages, combined with international pharmaceutical companies’ drug resources, to jointly develop the Middle East market.” This approach is particularly encouraged by Middle Eastern governments as it drives local healthcare industry growth and facilitates policy support.
Case Study: Collaboration between Middle Eastern Diagnostic Company Bait Al Dawaa and Novartis on Rare Diseases
Bait Al Dawaa, one of the largest local diagnostic companies in the Middle East, operates over 50 laboratories and more than 200 testing sites across the UAE, Saudi Arabia, Qatar, and other countries. It possesses deep familiarity with local regulatory frameworks and hospital procurement processes, granting it significant local channel advantages.Novartis developed a gene therapy for rare diseases like spinal muscular atrophy but faced challenges in the Middle East market, including insufficient distribution channels and difficulties in patient screening.
Their collaborative process is as follows:
- Establishing a “Rare Disease CDx Testing Network” (2023): Novartis provides CDx technical support for rare diseases (e.g., testing methods, reagent standards), while Bait Al Dawaa builds a specialized rare disease CDx testing network across the Middle East. “Rare Disease Testing Centers” are established in laboratories across 10 core cities to conduct patient screening and testing.
- Patient Registration and Treatment Coordination (2023-2024): Bait Al Dawaa leverages its channels to conduct rare disease screening campaigns. Patients meeting treatment criteria through CDx testing are registered in Novartis’ “Patient Treatment Database.” Novartis provides drug therapy for these patients and collaborates with Middle Eastern governments to include medications in national health insurance reimbursement lists;
- Long-term follow-up and data feedback (ongoing): Bait Al Dawaa conducts post-treatment follow-up testing and shares results with Novartis to optimize drug efficacy. Both parties jointly submit “Rare Disease Treatment Effectiveness Reports” to Middle Eastern governments to secure additional policy support (e.g., increased reimbursement rates, testing cost subsidies).
The model’s strength lies in its “grounded, actionable” approach: Local diagnostic companies understand regional markets, swiftly addressing “patient location, screening methods, and testing implementation.” International pharmaceutical firms provide high-quality drug resources to meet patient needs. Moreover, this “local + international” collaboration facilitates government policy support (e.g., insurance coverage, expedited approvals).
Implementation Key Points:
- Define “Responsibility Division”: Local diagnostics firms focus on channel development, patient screening, testing implementation, and regulatory compliance; international pharmaceutical companies concentrate on drug supply, technical support, and insurance negotiations—avoiding collaboration chaos caused by unclear responsibilities.
- Prioritize “Patient Education”: Many rare disease patients in the Middle East lack awareness about their conditions and treatments. Joint patient education initiatives (e.g., free clinics, educational seminars) are essential to boost screening willingness and treatment adherence.
- Establish Long-Term Partnerships: This model requires a longer implementation cycle (typically 1-2 years). Both parties must commit to sustained collaboration rather than pursuing short-term gains—for instance, agreeing to a minimum 5-year cooperation period and jointly investing resources in market cultivation.
Finally, a critical reminder: When pursuing “diagnostic-drug” collaborations in the Middle East market, it is essential to “closely follow government policies.”For instance, Saudi Arabia’s “Vision 2030” initiative emphasizes “enhancing access to precision medicine,” offering expedited approval channels for “diagnostic-drug” combination products. The UAE’s “Healthcare Industry Development Plan” provides financial subsidies for collaborative projects between local and international enterprises. Aligning collaborative projects with government policies not only accelerates approvals but also secures policy support and reduces operational costs.
Take the earlier example of Bait Al Dawaa and Novartis’ collaboration: they applied for Saudi Arabia’s “Precision Medicine Innovation Grant,” securing $2 million in funding to establish a rare disease testing network—accelerating their project timeline while reducing costs.
In summary, the scaling revolution of CDx fundamentally reflects the expansion of precision medicine beyond oncology into broader disease areas, with “diagnostic-drug” collaborations serving as the core pathway to achieve this scale.For pharmaceutical and diagnostics companies attending the conference, selecting the right collaboration model tailored to their needs, combined with the market demands and policy advantages of the Middle East, will enable them to seize the initiative in this revolution. After all, the Middle East’s CDx market is still growing rapidly, and entering now still offers significant market potential.

III. The Second Major Strategic Transformation Highlighted at 2026 Bio International Convention: Platformization and Democratization of Precision Medicine
3. Exclusive Perspective: Precision Medicine as the Key to Achieving “Value-Based Healthcare” in Emerging Markets
Historically, precision medicine carried an “exclusive and high-end” image—either as prohibitively expensive gene therapies for rare diseases or as genetic sequencing accessible only to top-tier hospitals, seemingly out of reach for ordinary individuals.However, Medlab 2026 conveyed a fundamentally different message: Precision medicine is shedding its “niche luxury” label, shifting toward “platforming” and “democratization.” This transformation is particularly evident in emerging markets like the Middle East.
Why emerging markets? Because regions like the Middle East face a core contradiction: on one hand, healthcare demand is exploding—an aging population, high prevalence of chronic diseases, and growing demand for high-end medical tourism, with people becoming increasingly discerning about “precise, effective” treatment plans; on the other hand, healthcare resources are limited—high-quality doctors and large hospitals are mostly concentrated in core cities like Dubai and Abu Dhabi, while remote areas lag in medical standards, and overall healthcare costs are rising.
This is where precision medicine emerges as the solution: by combining “precise diagnosis with personalized treatment,” it maximizes therapeutic outcomes while avoiding wasteful spending on ineffective care—the very essence of “value-based healthcare.” Consider cancer treatment: previously, patients might endure multiple costly and painful chemotherapy regimens with uncertain results. Now, genetic testing identifies targetable mutations, enabling direct use of targeted therapies that deliver superior efficacy while reducing unnecessary expenses.
Middle Eastern governments have long recognized this, making precision medicine a cornerstone of national strategies like “Vision 2030” and “Digital UAE.”Their goal isn’t “precision medicine accessible only to the few,” but rather precision medicine that “reaches more people, extends to grassroots levels, and lowers overall healthcare costs”—this is the core demand for “universalization.” Achieving universalization requires more than individual companies or technologies; it demands building a “platform-based” ecosystem: unified genetic databases, shared testing platforms, and collaborative industrial chains that enable SMEs and grassroots hospitals to participate.
At the 2024 Medlab exhibition, I spoke with an official from Saudi Arabia’s Ministry of Health who stated: “We don’t want precision medicine confined to top hospitals in Riyadh. Our vision is for every province in Saudi Arabia to offer genetic testing and personalized treatment. Achieving this requires transforming precision medicine into an ‘open platform’ where equipment manufacturers, testing institutions, pharmaceutical companies, and research institutes can collaborate.”
This encapsulates the “platformization + democratization” transformation Medlab 2026 will focus on: precision medicine shifting from “isolated breakthroughs” to “ecosystem synergy”; evolving from “elite exclusivity” to “universal accessibility.” Next, we’ll break down how this transformation materializes and identify tangible opportunities for attendees through three key directions: NGS technological breakthroughs, multi-omics integration, and the nucleic acid therapeutics/CGT industrial chain.
3.1 Breakthroughs in “Speed and Cost” of Next-Generation Sequencing (NGS)
NGS serves as the “core engine” of precision medicine—essential for genetic testing, disease screening, and drug development alike. The key to achieving widespread adoption in the Middle East lies in two factors: speed and cost. Previously, NGS sequencing was slow and expensive, limiting its use to research or select severe cases. Now, with increasing speed and decreasing costs, it has laid the foundation for integration into routine diagnostics and broader population coverage.
3.1.1 Cost Reduction Drives Whole Genome Sequencing (WGS) into Routine Diagnostics
First, consider these striking figures: the cost trajectory of whole-genome sequencing (WGS). By comparing global average costs from 2000 to 2024 with actual Middle Eastern market rates, the rationale for WGS’s diagnostic adoption becomes clear:
| Time Point | Global Average WGS Cost | Average WGS Fee in Middle East Market | Key Technology Breakthrough | Middle East Market Application Scenarios |
| 2000 | $100 million per person | – (No commercial services available) | First-generation sequencing technology, extremely low efficiency | Used exclusively for research; fewer than 10 cases globally |
| 2010 | $100,000 per person | $150,000 per person | Second-generation sequencing technology (Illumina platform) matured | Used exclusively for rare disease diagnosis, with annual testing volume under 100 cases |
| 2018 | $1,000 per person | $3,000 per person | Sequencer throughput increased, reagent costs decreased | Precision cancer therapy, rare disease screening, annual testing volume approximately 5,000 cases |
| 2024 | $200–300 per person | $800–1200 per person | Third-generation sequencing technologies (PacBio, Oxford Nanopore) become widespread; domestic companies introduce low-cost solutions | Routine diagnostics (e.g., cancer, cardiovascular diseases), newborn screening, and health checkups, with annual testing volume exceeding 50,000 cases |
| 2026 (Projected) | $100 per person | $500 per person | Portable sequencers achieve mass adoption; automated sample processing technologies mature | Routine testing at primary care hospitals and large-scale population screening, with annual testing volume projected to exceed 150,000 cases |
This table demonstrates that WGS costs have decreased by 500,000-fold over two decades—an unprecedented pace in any industry!While Middle Eastern market pricing remains above the global average (primarily due to local service and compliance costs), the downward trend aligns perfectly—reaching $800–1,200 per person by 2024. This price point is now within reach for the region’s middle-income population and aligns with government healthcare reimbursement capabilities.
This cost reduction has directly propelled WGS into routine diagnostics. Let me share two real-world examples from the Middle East market illustrating how WGS transitioned from a “niche test” to a “routine procedure”:
Case 1: Rashid Hospital in Dubai incorporates WGS into routine oncology diagnostics
Rashid Hospital, one of Dubai’s largest public hospitals, previously performed only “hotspot gene panel testing” (e.g., targeting common mutations like EGFR and ALK) for cancer patients at a cost of approximately $500. However, this approach had a critical limitation: it covered only a limited number of targets, often missing rare mutations and preventing some patients from identifying suitable targeted therapies.
In 2023, they incorporated WGS into routine cancer diagnostics—all confirmed advanced-stage cancer patients can now receive WGS free of charge (covered by Dubai government healthcare).Why was this possible? The key factor was cost reduction: In 2021, their WGS cost was $2,000 per person. By 2023, through bulk purchasing sequencing services from local companies, the cost dropped to $800 per person—fully affordable under government healthcare.
The impact has been significant: Previously, only 30% of advanced cancer patients could find matching targeted therapies; now that rate has risen to 55%. Moreover, by identifying rare targets, many patients have gained access to “orphan drugs,” extending their average survival by 12 months.More importantly, WGS predicts patient tolerance to chemotherapy drugs, avoiding wasted costs and side effects from ineffective treatments. Hospital statistics show that after implementing WGS, the average treatment cost for cancer patients decreased by 18%—a clear demonstration of value-based healthcare.
Case Study 2: Saudi Arabia’s Newborn WGS Screening Program
Saudi Arabia has a high incidence of rare diseases (due to a high rate of consanguineous marriages). Previously, newborn screening could only detect over 50 common genetic disorders, meaning many rare diseases were only diagnosed after symptoms appeared, missing the optimal treatment window.
In 2024, the Saudi government launched the “Newborn WGS Screening Pilot Program.” Maternity hospitals in five cities, including Riyadh and Jeddah, now offer free WGS screening for newborns—parents voluntarily enroll, with the government covering all costs (approximately $1,000 per person). The pilot aims to screen over 100,000 newborns for more than 1,000 rare diseases.
The project’s implementation hinges on breakthroughs in cost and speed: Previously, testing for 1,000 rare disease-related genes required multiple panel tests costing over $3,000 with results taking two weeks. Now, WGS completes the process in a single test, reducing costs to under $1,000 and delivering results within 72 hours.As of October 2024, the pilot program has screened 30,000 newborns, identifying 87 rare disease cases. All affected infants received timely treatment, preventing disease progression.
Some may wonder: “With such a significant cost reduction, does the accuracy of testing suffer?” In fact, there is no cause for concern.Modern NGS technology, particularly third-generation sequencing, not only offers lower costs but also achieves higher accuracy than previous methods. For instance, PacBio’s HiFi sequencing boasts an accuracy rate of 99.9%, surpassing second-generation sequencing. Moreover, it can detect structural variations (such as gene segment insertions or deletions) that were previously undetectable—variations often closely linked to rare diseases and tumors.
At the 2024 exhibition, Illumina showcased its latest NovaSeq X Plus sequencer. This instrument can complete WGS testing for 200 individuals within 24 hours, achieving an accuracy rate of 99.8% at an average cost of less than $200 per person.Meanwhile, Middle Eastern company PureHealth introduced its self-developed low-cost WGS solution. By partnering with local reagent suppliers, they reduced testing costs to $800 per person while offering database interpretation tailored specifically for Arab populations. This approach better aligns with local needs than international solutions, as genetic frequencies vary across populations, necessitating localized interpretation databases.
Another key driver for WGS adoption is government policy support. Middle Eastern governments not only cover WGS testing costs under healthcare insurance but are also building “national genomic databases.” For instance, the UAE’s “National Genomics Initiative” aims to collect genetic data from one million UAE citizens to establish a local population reference database.Saudi Arabia’s “Rare Disease Genetic Database” has already cataloged genetic data from 50,000 rare disease patients. These databases significantly enhance the accuracy and efficiency of WGS interpretation, enabling its practical application in routine diagnostics.
For attendees, this signifies a massive market opportunity: As WGS enters routine diagnostics, demand for NGS equipment, reagents, and interpretation services in the Middle East will explode.For instance, reagent production costs remain high locally in the Middle East, with many hospitals still relying on imports. This presents a prime market entry opportunity for reagent companies from China and Europe. Similarly, the region faces a shortage of bioinformaticians, necessitating third-party interpretation platforms—a gap that AI interpretation companies can fill.
3.1.2 The Rise of “Pocket Diagnostics”: Portable POCT Gene Sequencing Challenges Traditional Large-Scale Sequencing Centers
While the declining cost of WGS addressed the “feasibility” question, portable POCT gene sequencing solves the “accessibility” issue—it brings gene sequencing from “large laboratories” into “primary care clinics, emergency rooms, and remote areas,” serving as another key driver for the “democratization” of precision medicine.
First, a plain-language explanation: What is POCT gene sequencing? POCT stands for “Point-of-Care Testing,” meaning “on-site testing with rapid results.”Traditional sequencing required large-scale centers with dedicated labs and specialized operators. Samples had to be shipped for testing, yielding results days later. POCT sequencing devices, however, are as compact as microwaves—or even smaller. They require no specialized facilities and can be operated by primary care physicians. Results emerge within 1-2 hours after sample collection, giving rise to the term “pocket diagnostics.”
At the 2024 Medlab exhibition, POCT gene sequencing booths drew massive crowds, with numerous Middle Eastern primary care hospital and clinic administrators seeking information. The underlying demand is clear: they require “compact, user-friendly, rapid-result” genetic testing solutions to serve remote areas and emergency scenarios.
Let’s compare the core differences between traditional large-scale sequencing centers and POCT gene sequencing, examining their respective strengths, weaknesses, and suitable applications:
| Comparison Dimensions | Traditional Large-Scale Sequencing Centers | Portable POCT Gene Sequencing | Alignment with Core Middle Eastern Market Needs |
| Equipment Size | Large equipment (occupying 50-100 square meters), multiple units combined | Compact equipment (1-2 square meters footprint), integrated design | POCT better aligns with space constraints in primary care clinics and remote areas across the Middle East |
| Operational Complexity | Requires professional bioinformaticians and laboratory technicians | Primary care physicians can operate after 1-2 days of training | Addresses Middle East’s skilled personnel shortage, facilitating broader adoption |
| Testing Speed | Standard testing: 3-7 days for results; expedited: 24-48 hours | Results available within 1-2 hours | High demand in emergency and primary care settings (e.g., rapid diagnosis of infectious diseases) |
| Testing Cost (per test) | WGS: $800–1200; Panel testing: $300–500 | Panel testing: $100–200; select single-gene tests: $50 | Primary care market is price-sensitive; POCT holds greater advantage |
| Testing scope | Whole genome, whole exome, large panel testing (covering thousands of genes) | Small panel testing (covering dozens of genes), single-gene testing | Routine diagnostics and emergency scenarios often require targeted testing, which POCT can sufficiently cover |
| Applicable Scenarios | Large hospitals, research institutions, rare disease diagnosis, multi-gene disease screening | Primary care clinics, emergency rooms, remote areas, rapid infectious disease diagnosis, chronic disease follow-up | The Middle East is driving the decentralization of healthcare resources, expanding the applicability of POCT. |
As this table illustrates, POCT gene sequencing is not intended to replace traditional large-scale sequencing centers but to complement them—large centers handle “comprehensive, in-depth” testing (e.g., WGS, rare disease diagnosis), while POCT manages “rapid, convenient” testing (e.g., emergency infectious disease diagnosis, primary care chronic disease screening). Only through this integration can precision medicine achieve comprehensive coverage.
Here are two real-world examples from the 2024 exhibition showcasing how POCT gene sequencing is being implemented in the Middle East:
Case 1: Oxford Nanopore’s MinION sequencer in Dubai emergency rooms
At Dubai’s Rashid Hospital emergency department, patients presenting with “fever of unknown origin” previously posed challenges in rapidly distinguishing bacterial from viral infections. This often led to empirical antibiotic use—potentially contributing to antibiotic overuse while delaying treatment for viral infections.
In 2023, they introduced Oxford Nanopore’s MinION sequencer (a palm-sized POCT gene sequencing device) for rapid emergency diagnosis of infectious diseases. The specific workflow is as follows:
- After drawing blood from the patient, use the accompanying rapid nucleic acid extraction kit (completed in 15 minutes);
- The extracted nucleic acid sample is loaded into the MinION sequencer, selecting the “Infectious Disease Detection Panel” (covering over 50 common pathogens and viruses);
- After 1.5 hours, the device automatically outputs results such as “COVID-19 detected, no common bacteria detected” or “Streptococcus pneumoniae detected, penicillin-class antibiotics recommended.”
Implementation yielded significant outcomes: Emergency infectious disease diagnosis accuracy rose from 75% to 92%; antibiotic overuse decreased by 30%; average patient hospital stays shortened by 1.2 days. For hospitals, this not only enhances diagnostic quality but also reduces operational costs. For patients, it enables rapid, precise treatment while avoiding unnecessary medication.
Crucially, the device is exceptionally user-friendly: emergency nurses can independently complete the entire process from sample handling to testing after just one day of training, eliminating the need for bioinformaticians—perfectly addressing the Middle East’s shortage of specialized personnel.By 2024, ten public hospital emergency rooms in Dubai had adopted this technology. The government plans to equip all secondary and higher-level hospital emergency rooms with POCT gene sequencing devices by 2025.
Case Study 2: Bayanat and PureHealth’s “POCT Solution for Primary Care Chronic Disease Screening”
Chronic diseases like hypertension and diabetes have high prevalence rates in the Middle East, yet primary care clinics lack precise screening tools. Currently, they can only make preliminary assessments through blood pressure and blood glucose tests, unable to predict complication risks.
Bayanat (an Abu Dhabi-based AI company) partnered with PureHealth to launch a POCT gene sequencing device for chronic diseases. About the size of a microwave oven, it can detect over 20 genetic loci associated with hypertension and diabetes complications. The test costs only $100 per person and delivers results within one hour.
The device’s core advantage lies in “localized interpretation”: it integrates a genetic database of Arab populations to provide personalized chronic disease management recommendations based on individual test results. For example: “The patient carries an ABCA1 gene variant, indicating higher risk of diabetic nephropathy. Renal function tests are recommended every 6 months.” Or: “The patient carries an ADRB1 gene variant, showing sensitivity to beta-blocker antihypertensive drugs. Priority use is advised.”
In 2024, this device underwent pilot testing in 50 primary care clinics across the UAE, covering 20,000 chronic disease patients.Pilot data revealed that after implementing POCT genetic testing, the rate of patients achieving target chronic disease control improved from 58% to 76%, while complication incidence decreased by 22%. This improvement stems from patients being able to adjust medication and lifestyle based on genetic test results, enabling personalized chronic disease management.
Of course, POCT gene sequencing faces challenges: limited testing scope (cannot perform whole-genome sequencing); room for improvement in detection accuracy for complex samples (e.g., blood samples with low pathogen concentrations); and data processing/storage must comply with Middle Eastern healthcare data security standards.
However, these challenges are being rapidly addressed: At the 2024 exhibition, Illumina launched a new POCT sequencer with a testing panel covering over 100 genes and accuracy improved to 99.5%. Furthermore, many companies have introduced “cloud-based data management platforms” where data from POCT devices is automatically uploaded to the cloud for secondary interpretation by professional teams. This approach not only addresses talent shortages at the grassroots level but also ensures data security.
For attendees, POCT gene sequencing presents a “low-barrier, high-growth” opportunity:
- For device manufacturers: Prioritize developing “compact, user-friendly, localized” POCT devices, especially for infectious diseases, chronic conditions, and newborn screening—the Middle East’s primary healthcare market is rapidly expanding with massive demand.
- If you are a reagent supplier: Develop complementary rapid, low-cost consumables like nucleic acid extraction kits and detection probes—POCT device consumables represent sustained demand with high replacement rates;
- If you are a service provider: Establish a “POCT Data Interpretation Cloud Platform” to offer secondary interpretation services for primary care clinics—this addresses the Middle East’s talent shortage and presents substantial market potential.
3.2 From Genomics to Multi-Omics
If NGS solved the “tool problem” for precision medicine, multi-omics addresses its “depth problem.” Previously, focusing solely on genomics was like “reading only a book’s table of contents”—it provided general direction but obscured details.Multi-omics, however, is like “reading the entire book.” By integrating data from multiple dimensions—genomics, transcriptomics, proteomics, metabolomics, and more—we can achieve a more comprehensive and precise understanding of disease mechanisms, enabling personalized treatment plans.
3.2.1 AI-Empowered Data Fusion: The Necessity of Integrating Multi-Omics Data
First, let me clarify what these “omics” disciplines are and what problems each addresses—many people tend to confuse them, so I’ll use a straightforward table to explain:
| Type of Omics | Core Research Object | Layman’s Explanation | Role in Precision Medicine | Limitations When Used Alone |
| Genomics | The Entire Genome (DNA) | The Human “Genetic Blueprint” | Predicts disease risks (e.g., tumors, rare diseases) and guides targeted drug selection | Can only assess “inherited risk,” not acquired changes (e.g., whether genes are activated) |
| Transcriptomics | Transcripts of genes (RNA) | The “interpretation records” of the code book | Determines whether genes are activated and the extent of activation | Can only reflect gene expression patterns, not protein function |
| Proteomics | All proteins | Functional machinery synthesized according to the genetic code | Directly reflects cellular functional states (e.g., abnormal protein expression in tumor cells) | Proteins are prone to degradation, making detection challenging with high data variability |
| Metabolomics | Metabolic byproducts (e.g., glucose, amino acids) | “Waste/products” generated during machine operation | Reflects disease progression (e.g., metabolic disorders in diabetes) and treatment efficacy | Susceptible to external factors like diet and exercise, with relatively low specificity |
| Microbiomics | Microorganisms in the human gut, skin, etc. | The human “symbiotic microbial community” | Influences chronic diseases (e.g., obesity, diabetes) and immune function | Complex microbial composition, highly influenced by environment, challenging to interpret |
This table illustrates the limitations of individual omics data—for instance, genomics can predict tumor risk but cannot determine if that risk is active; proteomics can detect abnormal tumor proteins but cannot identify the causative genes. Only by integrating these data can we form a “complete disease profile.”
Consider this example: A patient suspected of lung cancer undergoes genomic testing alone, revealing an EGFR gene mutation. This indicates potential sensitivity to EGFR-targeted drugs but leaves unanswered questions about tumor progression and the patient’s immune tolerance to treatment. Transcriptomic testing then shows elevated EGFR gene RNA expression (indicating gene activation). Proteomic testing detects EGFR protein overexpression.and metabolomics testing reveals elevated tumor-associated metabolites—this forms a complete chain of evidence. Physicians can not only confirm the use of targeted drugs but also determine dosage, predict treatment efficacy, and even anticipate side effects in advance.
Manually integrating multi-omics data is utterly impossible—each omics generates massive datasets (e.g., a single human genome contains 3 billion base pairs). The combined volume becomes “big data,” requiring AI technology for processing, analysis, and fusion.
At the 2024 Medlab Exhibition, AI-enabled multi-omics data integration emerged as one of the hottest topics, with numerous companies showcasing related solutions. Let’s examine a Middle Eastern case study to illustrate how AI integrates multi-omics data:
Case Study: The “Precision Diabetes Diagnosis and Treatment Multi-omics AI Platform” developed by Mohamed bin Zayed University of the UAE in collaboration with IBM
Diabetes is a highly prevalent chronic disease in the Middle East, with many patients developing complications like kidney disease and retinopathy. Traditional diagnostics rely solely on blood glucose monitoring to adjust medication, lacking the ability to accurately predict complication risks.
This collaborative project established a multi-omics AI platform centered on the following approach:
- Data Collection:Collected multi-omics data from 10,000 diabetes patients—genomics (analyzing over 50 diabetes-related genes), metabolomics (analyzing over 100 metabolites), proteomics (analyzing over 80 diabetes-related proteins), and microbiomics (gut microbiota data)—alongside clinical data (blood glucose, blood pressure, medication history) and lifestyle data (diet, exercise, sleep).;
- AI Model Training: Using IBM’s Watson AI platform, we trained a “Complication Risk Prediction Model” and a “Personalized Treatment Recommendation Model”——AI automatically identifies correlations between multi-omics data and complications. For example, patients with “TCF7L2 gene mutation + low Bifidobacterium ratio in gut microbiota + high glycated hemoglobin in metabolites” face a 5-fold higher risk of kidney disease compared to average patients;
- Clinical Application: When clinicians input a patient’s multi-omics and clinical data, the AI generates within 10 minutes a “Complication Risk Score” (e.g., 85% risk of kidney disease, 30% risk of retinopathy) and “Personalized Treatment Recommendations” (e.g., “Recommend SGLT-2 inhibitor hypoglycemic agents to reduce kidney disease risk; concurrently supplement with probiotics to regulate gut microbiota”).
Following pilot implementation across 10 hospitals in the UAE, the platform demonstrated remarkable outcomes: Complication prediction accuracy for diabetic patients increased from 62% to 88%;Intervention rates for high-risk patients rose from 45% to 78%; complication incidence decreased by 25%; and average treatment costs per patient fell by 22%. This exemplifies the core value of AI-enabled multi-omics data fusion: elevating precision medicine from “accurate diagnosis” to “accurate treatment and prognosis.”
Another international example is the “Tumor Multi-Omics AI Interpretation Platform” developed through collaboration between Roche Diagnostics and Google DeepMind.This platform integrates tumor patients’ whole-genome sequencing (WGS) data, proteomics data, and imaging data (such as CT and MRI). AI automatically identifies tumor driver genes, mutation patterns, and protein expression characteristics, and can even detect microscopic tumor lesions invisible to the naked eye from imaging data. It then provides an integrated solution comprising “diagnostic reports + treatment recommendations + prognosis assessments.”
In 2024, this platform was deployed at Cleveland Clinic in Dubai for precision diagnosis and treatment of advanced cancer patients. Hospital statistics indicate that its implementation increased targeted drug matching accuracy by 30%, boosted immunotherapy response rates by 25%, and extended median patient survival by 9 months.
AI-enabled multi-omics data fusion offers another critical advantage: uncovering “novel disease mechanisms.” For instance, while a specific gene mutation was previously unlinked to diabetic nephropathy, AI analysis of multi-omics data revealed its strong correlation with particular protein expression and metabolite changes—unveiling a new disease pathway. This provides novel targets for drug development and continuously deepens the “depth” of precision medicine.
For attendees, this signifies two core opportunities:
- First, the “AI Tool Opportunity”: The Middle East lacks AI platforms capable of processing multi-omics data, particularly localized platforms (requiring adaptation to Arab populations). If your company can provide “multi-omics data integration AI tools”—including functions like data cleaning, feature extraction, model training, and result interpretation—they will be highly sought after by hospitals and research institutions.
- Second, the “Data Service Opportunity”: Many small-to-medium laboratories and primary-care hospitals lack the capacity to collect and process multi-omics data, necessitating third-party services. Offering integrated “multi-omics data detection + AI interpretation” services—such as multi-omics screening packages for chronic disease patients or precision diagnostics/therapeutics for cancer patients—presents substantial market potential.
3.2.2 Core Pain Points and Solutions: Bioinformatics Talent Shortage and Data Analysis Platform Selection
Although the convergence of multi-omics and AI is a trend, its implementation in the Middle East market faces a major pain point: the shortage of bioinformatics talent. Without sufficient talent, even the best technology and the most data cannot be effectively utilized.
Consider these alarming statistics: According to the Middle East Healthcare Technology Association (META) 2024 report, the region faces an 80% shortage of bioinformatics professionals, as detailed below:
| Middle East Region | Bioinformatics Talent Demand (2024) | Current Talent Pool | Shortfall | Shortage Ratio | Regions with Highest Concentration of Talent |
| United Arab Emirates | 3,000 people | 650 people | 2,350 people | 78.3% | Dubai, Abu Dhabi |
| Saudi Arabia | 5,000 people | 900 people | 4,100 people | 82.0% | Riyadh, Jeddah |
| Qatar | 800 people | 150 people | 650 people | 81.2% | Doha |
| Other GCC Countries | 2,200 people | 350 people | 1,850 | 84.1% | Kuwait City, Muscat |
| Total | 11,000 people | 2,050 | 8,950 people | 81.4% | Concentrated in core cities, virtually nonexistent at the grassroots level |
Why such a significant gap? Three primary reasons:
- Lagging education system: Most universities in the Middle East do not offer bioinformatics programs. Only a handful of top institutions (such as Mohamed bin Zayed University and King Saud University) provide relevant courses, producing fewer than 200 graduates annually—far short of demand.
- Severe talent drain: Many locally trained bioinformaticians migrate to Europe or the United States for higher salaries and better research environments, leading to a retention crisis for Middle Eastern talent.
- Explosive demand growth: With the widespread adoption of multi-omics and NGS, demand for bioinformatics talent is surging rapidly. However, the lengthy training cycle (typically 5-10 years) exacerbates the supply-demand imbalance.
What are the direct consequences of this gap? At the 2024 exhibition, I heard a Middle Eastern laboratory director lament: “Last year we purchased a multi-omics testing system and collected data from 500 patients. But without bioinformaticians, this data just sits dormant on our servers—utterly unusable. We spent millions on equipment that’s now just a decoration.”
Another Chinese company supplied NGS equipment and an AI interpretation platform to a Saudi hospital. However, the hospital lacked bioinformaticians trained to use the platform, forcing them to rely on remote support from Chinese experts. This not only incurred high communication costs but also frequently delayed reports due to time zone differences and language barriers, ultimately resulting in low hospital satisfaction.
Therefore, for attendees looking to pursue multi-omics-related business in the Middle East, addressing the “talent gap” is the critical pain point. The solution lies not in “cultivating talent internally” (which takes too long), but in “selecting the right data analysis platform.” This approach allows the platform to replace some of the work traditionally done by specialists or reduce the specialized expertise required.
Below, I outline the three main types of data analysis platforms currently available in the Middle East market, along with their respective pros and cons, suitable scenarios, and selection recommendations for your direct reference:
Category 1: Cloud-Based Integrated Data Analysis Platforms (Representative Companies: Illumina BaseSpace, IBM Watson for Genomics)
These platforms offer a “one-stop solution”—handling everything from data upload, cleaning, and analysis to result interpretation and report generation entirely in the cloud. Users need neither to set up servers nor hire specialized bioinformaticians; basic computer skills suffice for operation.
Core Advantages:
- User-friendly operation: Visual interfaces simplify workflows. For example, after uploading NGS raw data, users select a relevant testing panel (e.g., oncology, rare diseases), and the platform automatically analyzes the data, generating standardized reports within 1-2 hours.
- Zero Maintenance: Server management, software updates, and database upgrades are handled by the platform provider, eliminating the need for dedicated IT personnel.
- Robust Databases: Integrates major global gene databases (e.g., ClinVar, OMIM), with some platforms incorporating Middle Eastern databases (e.g., UAE National Genome Database), ensuring high interpretation accuracy.
Core Disadvantages:
- Data security concerns: Some hospitals worry about patient data leakage when uploaded to the cloud—though platforms employ encryption measures, Middle Eastern countries have extremely stringent medical data privacy requirements. Certain government agencies (e.g., Saudi Arabia’s SFDA) prohibit the transfer of sensitive data outside the country.
- Higher Costs: Pay-per-use pricing models apply, e.g., WGS data analysis costs approximately $100–200 per run, resulting in significant long-term expenses.
- Limited customization: Only standardized analysis reports are provided, failing to meet research institutions’ needs for personalized analysis (e.g., custom gene panels, specialized data analysis algorithms).
Suitable scenarios: Primary care clinics, small-to-medium hospitals, and institutions without bioinformatics expertise—for example, primary care clinics in the Middle East can upload data to cloud platforms and generate reports quickly after purchasing POCT sequencing equipment, without requiring specialized personnel.
Selection Recommendations:
- Prioritize platforms with “local servers in the Middle East”—e.g., Illumina operates a local cloud node in Dubai, storing data locally to meet compliance requirements;
- Verify whether the platform offers “localized interpretation capabilities”—such as incorporating genetic frequency data for Arab populations and providing reports in Arabic (many primary care physicians in the Middle East speak only Arabic).
Category 2: On-Premises Data Analysis Platforms (Representative Vendors: QIAGEN CLC Genomics Workbench, Thermo Fisher Ion Torrent Suite)
These platforms require installation on the user’s own servers, with data storage and analysis conducted locally. They provide basic analytical tools and templates, necessitating 1-2 personnel with foundational bioinformatics skills for operation and maintenance.
Core Advantages:
- Data Security: Data remains entirely within local storage, complying with Middle Eastern healthcare privacy regulations. Government agencies and large hospitals prefer this option.
- High Customizability: Analysis workflows, gene panels, and report templates can be tailored to user requirements—e.g., research institutions can design multi-omics data integration algorithms, while large hospitals can adjust report content based on their clinical protocols;
- Low Long-Term Costs: A one-time software license purchase requires only maintenance fees thereafter, making it suitable for high-volume testing facilities (e.g., annual throughput exceeding 1,000 cases).
Core Disadvantages:
- High barrier to entry: Requires users to set up their own servers (hardware investment of approximately $50,000–100,000 USD) and employ 1–2 bioinformatics personnel for operation—though the professional requirements are lower than traditional analysis tools, basic expertise is still necessary;
- Complex maintenance: Requires IT personnel for server upkeep and software updates. Technical support issues may involve contacting the platform provider, potentially with slower response times compared to cloud-based platforms.
Suitable Scenarios: Large hospitals, research institutions, and high-volume testing laboratories—such as Dubai’s Rashid Hospital, which processes over 5,000 tests annually. On-premises deployment ensures data security while meeting customization needs.
Selection Recommendations:
- Verify platform “compatibility”—e.g., whether it supports data formats from multiple sequencing devices (e.g., Illumina, PacBio, Oxford Nanopore) and integrates multi-omics data (genomics, proteomics, metabolomics).
- Evaluate the platform provider’s “local technical support capabilities”—such as whether they maintain a technical service team in the Middle East and can respond to issues within 24 hours.
Category 3: Open-Source Data Analysis Platforms (Representative Companies: Galaxy, BWA, GATK)
These platforms are free and open-source, allowing users to download software, build analysis workflows, and fully customize analytical solutions—ideal for research institutions with specialized bioinformatics teams requiring deep customization.
Core Advantages:
- Completely free: The software itself is free with no usage limits, offering the lowest long-term cost;
- Highly Customizable: Freely combine analysis tools and design workflows based on research needs—e.g., integrating multi-omics data with custom algorithms to identify novel gene targets for rare diseases;
- High Flexibility: Analysis workflows can be optimized based on user server configurations to enhance processing speed.
Core Disadvantages:
- High Barrier to Entry: Requires a professional bioinformatics team (minimum 2-3 members) proficient in both data analysis and programming (e.g., Python, R) to build and maintain analysis workflows;
- Lack of standardized support: No official technical support is available; issues must be resolved through community forums. Report generation requires custom template design and cannot be directly applied for clinical diagnosis.
- Database Integration Requirement: The open-source platform itself does not include gene databases; users must download and integrate them independently, with interpretation accuracy dependent on database completeness.
Suitable Scenarios: Universities, research institutions, and large enterprises with established bioinformatics teams—such as the Mohamed bin Zayed University of Science and Technology in the UAE, which utilizes the Galaxy platform for multi-omics research analysis through its dedicated bioinformatics laboratory.
Recommendations:
- Prioritize open-source platforms with “active communities”—for example, Galaxy hosts the world’s largest bioinformatics open-source community, enabling rapid problem-solving when issues arise;
- Verify if the platform offers “Middle East localized plugins”—some research institutions have developed analysis plugins tailored for Arab population genetic data, which can be directly integrated into open-source platforms to enhance analytical efficiency.
Here’s a real-world selection case: A medium-sized hospital in Saudi Arabia (processing approximately 800 tests annually) lacked bioinformatics expertise but required NGS testing for tumors and rare diseases. They ultimately chose Illumina’s BaseSpace cloud platform for these core reasons:
- Simple operation: Nurses could use it after training, eliminating the need to hire bioinformaticians;
- Illumina maintains a data center in Saudi Arabia, ensuring local data storage that complies with SFDA regulations;
- The platform includes a genetic database for Arab populations, ensuring high interpretation accuracy;
- Pay-per-use pricing with low initial investment, eliminating the need for server infrastructure.
Post-implementation, the hospital reduced NGS reporting time from 7 days to 2 days, increased monthly throughput from 50 to 80 cases, and achieved these gains without additional staffing costs—demonstrating the value of “selecting the right platform.”
A crucial reminder for attendees: When selecting a data analytics platform in the Middle East, “compliance” outweighs “functionality.” For instance, some platforms may offer robust features but require data to leave the country, making them ineligible for Saudi SFDA approval—no matter how effective they are. Therefore, always consult local regulatory authorities or engage partners with regional compliance expertise to verify platform adherence to local regulations before making a selection.
3.3 Building the Industrial Chain for Nucleic Acid Therapeutics and CGT (Cell and Gene Therapy)
Achieving precision medicine’s goals of “platformization” and “democratization” ultimately hinges on “treatment solutions”—and nucleic acid therapeutics and CGT represent the most core therapeutic approaches in precision medicine. Recognizing this sector’s potential, Middle Eastern governments are aggressively building out the industrial chain, presenting attendees with a rare “early-stage entry opportunity.”
3.3.1 Middle East/GCC Investment Opportunities: Regional Governments’ Strategic Investments in CGT Manufacturing and Clinical Trials
The Middle Eastern governments’ emphasis on nucleic acid therapeutics and cell and gene therapies (CGT) far exceeds common expectations—they are not merely seeking to “import therapies,” but rather to “build their own industrial chains.” This involves establishing a complete ecosystem spanning R&D, clinical trials, manufacturing, and commercialization. The underlying logic is straightforward: nucleic acid therapeutics and CGT represent high-value-added sectors capable of driving medical technology industry upgrades. Simultaneously, they address local treatment needs for rare and chronic diseases while attracting global medical tourism.
Let’s outline the strategic plans and investment activities of key Middle Eastern countries in a table for clarity:
| Country | Core Strategy | Investment Amount (2020-2025) | Key Focus Areas | Key Initiatives | Projects Already Implemented |
| United Arab Emirates | “Digital UAE” + “Medical Tourism Upgrade” | $8 billion | CGT Manufacturing, Clinical Trials, Nucleic Acid Drug R&D | 1. Established the “CGT Industrial Park” in Abu Dhabi, offering tax exemptions and expedited approvals;<br>2. Launched a $2 billion precision medicine fund to invest in nucleic acid therapeutics and CGT enterprises;<br>3. Signed mutual recognition agreements with the FDA and EMA, enabling clinical trial data to be used for global approvals | 1. Partnering with Novartis to establish CGT manufacturing base (commencing operations in 2024);<br>2. Abu Dhabi CGT Industrial Park has attracted 15 companies (including 3 Chinese firms);<br>3. Conducting 20 CGT clinical trials (primarily targeting rare diseases and oncology) |
| Saudi Arabia | Healthcare Sector of the “Vision 2030” | $12 billion | Rare disease CGT, nucleic acid drug manufacturing, gene therapy center | 1. Investing $5 billion to build 3 CGT manufacturing facilities;<br>2. Establishing a “Rare Disease Treatment Fund” to cover patient payments for CGT therapies;<br>3. Creating a national clinical trial network integrating resources from 20 public hospitals | 1. Collaborate with Bluebird Bio on sickle cell anemia CGT clinical trials;<br>2. Riyadh CGT manufacturing facility (commencing operations in 2025);<br>3. Five CGT therapies approved for market launch (including two domestically developed products) |
| Qatar | “Qatar National Health Strategy 2030” | $3 billion | Cancer CGT, nucleic acid drug R&D, biobank | 1. Investing $1 billion to establish the Qatar Precision Medicine Center;<br>2. Partnering with Mayo Clinic to build a clinical trial collaboration network;<br>3. Collecting biological samples from 500,000 citizens to establish the Middle East’s largest biobank | 1. Conducted 12 oncology CGT clinical trials;<br>2. Biobank has enrolled 200,000 samples;<br>3. Established nucleic acid drug R&D laboratory in partnership with AstraZeneca |
| Kuwait | “Kuwait National Development Plan 2035” | $2.5 billion | CGT distribution, localized production, patient access programs | 1. Construct a regional CGT logistics distribution center (covering GCC countries);<br>2. Offer a 15-year tax exemption policy for CGT enterprises;<br>3. Provide full health insurance coverage for rare disease CGT therapy costs | 1. Establishing a CGT cold chain logistics network in partnership with FedEx;<br>2. Introducing localized production of 3 CGT therapies;<br>3. 500 rare disease patients have already received CGT treatment |
This table reveals three core characteristics of Middle Eastern governments’ strategic initiatives:
- Massive investment scale: Total investment exceeds $25 billion, with substantial capital deployment rather than mere theoretical planning;
- Focus on Manufacturing and Clinical Trials: Prioritizing CGT manufacturing hubs and clinical trial networks—core segments of the industry chain that currently represent global bottlenecks (insufficient CGT manufacturing capacity and prolonged clinical trial cycles);
- Substantial Policy Incentives: Tax exemptions, expedited approvals, healthcare coverage, and fund support—these policies rapidly attract enterprises and accelerate industrial chain implementation.
Here’s a concrete example of an implemented project to illustrate how the Middle East is building its CGT industrial chain:
Case Study: Abu Dhabi CGT Park
This industrial park, a key CGT industry hub developed by the UAE government, is located in Abu Dhabi’s Khalifa Industrial Zone. With a total investment of $1.5 billion and covering 1 million square meters, its core advantage lies in its “one-stop ecosystem services.” Companies that establish operations here receive comprehensive support throughout the entire process—from R&D and clinical trials to manufacturing and commercialization:
- R&D Support: The park houses a dedicated “CGT R&D Center” equipped with advanced laboratory facilities. Companies can share equipment resources to reduce R&D costs. It also collaborates with UAE universities to provide talent support.
- Clinical Trial Support: Partnerships with five top-tier Abu Dhabi hospitals establish a clinical trial fast track—typically reducing CGT trial approvals from 6-12 months to just 3-6 months. Hospitals also provide patient resources to accelerate enrollment.
- Manufacturing Support: The industrial park offers standardized GMP production facilities, eliminating the need for companies to build their own plants—they can begin production immediately upon moving in. It also provides complementary services such as cold chain storage and quality testing.
- Policy Incentives: Tenant companies enjoy 15 years of tax exemption (full exemption from corporate income tax and VAT); imported equipment and reagents are duty-free; clinical trial data can be used for approvals by multiple agencies including the FDA, EMA, and HAAD.
- Market Access: The park collaborates with healthcare insurance agencies in GCC countries, enabling tenant products to rapidly enter their national reimbursement lists. It also partners with medical tourism companies to attract global patients for treatment.
As of October 2024, the industrial park has attracted 15 companies, including international giants like Novartis and Bluebird Bio, alongside three Chinese enterprises (one CGT equipment manufacturer and two reagent suppliers).Novartis’ CGT manufacturing facility has commenced operations, primarily producing Zolgensma therapy for spinal muscular atrophy. Its annual output meets the entire GCC region’s demand while enabling exports to Africa and South Asia.
Another noteworthy aspect is the Middle Eastern governments’ strong emphasis on “local R&D.” For instance, Saudi Arabia’s “Rare Disease Treatment Fund” not only supports patient care but also allocates 30% of its resources to fund local companies conducting CGT research and development.In 2024, the CGT therapy for sickle cell anemia developed by Saudi Arabia’s Naif Medical Research Center entered clinical trials—marking the Middle East’s first locally developed CGT therapy. The Saudi government has provided $200 million in funding for this project.
For attendees, these strategic initiatives present three major investment opportunities:
- Manufacturing Opportunities: Middle Eastern CGT manufacturing hubs require substantial equipment, reagents, and consumables—such as bioreactors, cold chain equipment, cell separation reagents, and gene editing tools. Currently, most of these products rely on imports. Chinese and European companies that secure supplier status can expect stable orders.
- Clinical Opportunities: The Middle East’s clinical trial network requires support from CROs (Contract Research Organizations) and SMOs (Site Management Organizations) for services like patient recruitment, clinical trial management, and data analysis. With few local Middle Eastern CRO/SMO firms, international companies have substantial market potential.
- Service Opportunities: Storage, logistics, and patient follow-up services for CGT therapies represent a significant gap in the Middle East. For instance, CGT therapies require end-to-end cold chain transportation, and the region’s high temperatures impose stringent logistics demands. Companies offering specialized cold chain logistics services will be highly sought after.
3.3.2 Value for Attendees: Positioning as Strategic Partners for Emerging Nucleic Acid Therapeutics Companies
The Middle East’s nucleic acid therapeutics and CGT industry chains are still rapidly developing. Many emerging local pharmaceutical companies and international firms entering the region are seeking strategic partners—presenting attendees with an exceptional opportunity for “early engagement.” Different attendee types should pursue distinct positioning strategies and collaboration models. Below is a detailed breakdown by category:
Type 1: Equipment/Reagent/Consumables Suppliers (e.g., sequencing instruments, bioreactors, cell separation reagents, gene editing tool providers)
These enterprises form the “foundational backbone” of the industrial chain and represent the most urgent demand in the Middle East market—as CGT manufacturing facilities and laboratories require substantial equipment and consumables, most of which are currently imported.
Cooperation Models and Layout Recommendations:
- Establish presence in industrial parks as “designated suppliers”: Middle Eastern CGT industrial parks (e.g., Abu Dhabi CGT Park) provide recommended supplier lists to resident companies. Securing a park residency or becoming a “designated supplier” enables direct access to pharmaceutical firms within the park.For example, a Chinese cell separation reagent supplier that entered the Abu Dhabi CGT Park in 2023 became a core supplier for Novartis and Bluebird Bio in the Middle East by 2024, achieving annual sales exceeding $50 million.
- Collaborating with local pharmaceutical companies for “localized production”: Middle Eastern governments encourage localized manufacturing. By partnering with local pharmaceutical firms to establish joint-venture factories in the region for producing equipment or consumables, companies can benefit from policies such as tax exemptions and priority procurement by public healthcare systems.For example, a European bioreactor supplier partnered with a Saudi pharmaceutical company to establish an assembly plant in Riyadh. Their products now supply not only the Saudi market but also export to other GCC countries, achieving a 20% cost reduction and rapid market share growth.
- Offer integrated “equipment + service” solutions: Middle Eastern pharmaceutical companies lack personnel skilled in equipment operation and maintenance. Providing comprehensive services encompassing “equipment sales + installation + training + after-sales maintenance” enhances competitiveness.For instance, a sequencing instrument supplier secured a bulk procurement order from the Qatari government by not only providing sequencing instruments to Qatar’s Precision Medicine Center but also deploying a technical team for a six-month on-site residency to train local operators, coupled with a commitment to 24-hour after-sales response.
Key Considerations:
- Must comply with GMP standards: Middle Eastern requirements for CGT-related equipment and reagents are stringent, necessitating GMP certification. Certain products also require registration with HAAD or SFDA.
- Adapt to local conditions: The Middle East’s high temperatures and humidity demand exceptional stability from equipment and reagents. For instance, cold chain reagents must withstand temperature fluctuations during transport, while equipment requires high-temperature protection features.
Type 2: CRO/CMO/CDMO Enterprises (Contract Research Organizations/Contract Manufacturing Organizations/Contract Development and Manufacturing Organizations)
These entities serve as the “core service providers” in the industry chain—most emerging pharmaceutical companies in the Middle East lack mature R&D and manufacturing capabilities, necessitating reliance on CRO/CMO/CDMO firms for services.
Cooperation Models and Layout Recommendations:
- Partner with clinical trial networks to undertake local trials: National clinical trial networks in the Middle East (e.g., Saudi Arabia’s National Clinical Trial Network) consolidate extensive hospital and patient resources. Becoming a network-affiliated CRO enables access to numerous CGT clinical trial projects.For example, a global CRO partnered with the UAE’s clinical trial network in 2022 and secured 8 CGT clinical trials in 2023-2024, generating over $100 million in revenue.
- Establishing CDMO Bases in Industrial Parks for Localized Manufacturing Services: Many international pharmaceutical companies seek to enter the Middle East market without building their own facilities, opting instead to partner with CDMO firms. For instance, a Chinese CDMO company established a production base in Abu Dhabi’s CGT Industrial Park, providing localized manufacturing services for CGT therapies to companies like Novartis and AstraZeneca, with capacity utilization already reaching 80%.
- Offering integrated “R&D + manufacturing“ services: For local Middle Eastern pharmaceutical startups lacking capital and resources, providing end-to-end services spanning drug development, clinical trials, and commercial production—these startups urgently require such “one-stop solutions.” For instance, a European CDMO firm delivered comprehensive services to a Saudi CGT startup, accelerating its therapy into clinical trials while securing equity dividends from the company.
Key Considerations:
- Familiarize with local regulations: Clinical trial regulations and approval processes in the Middle East differ from those in Europe and the US. For instance, Saudi Arabia’s SFDA imposes stricter ethical review requirements for CGT clinical trials, necessitating advance preparation.
- Establish local teams: Clinical trials demand extensive local coordination (e.g., patient recruitment, hospital liaison, ethics communication). Building a local team is essential for enhancing efficiency.
Type 3: Healthcare Service Providers (e.g., Hospitals, Clinics, Testing Centers)
These institutions serve as the “end-point implementation vehicles” in the industrial chain—nucleic acid drugs and CGT therapies must ultimately be administered to patients through hospitals, accompanied by complementary testing and follow-up services.
Collaboration Models and Strategic Recommendations:
- Becoming a “Designated CGT Therapy Center”: Partner with pharmaceutical companies to become their designated treatment hospital for CGT therapies, responsible for patient screening, treatment implementation, and long-term follow-up. For example, the Cleveland Clinic in Dubai partnered with Bluebird Bio to become the Middle East’s sole designated treatment center for its sickle cell anemia CGT therapy, attracting numerous patients from the Middle East and Africa and significantly boosting medical tourism revenue.
- Establish a “Precision Diagnosis and Treatment Integration Platform“: Integrate multi-omics testing, AI interpretation, CGT therapy, and follow-up management services to provide patients with “one-stop precision medical services.” For example, a private hospital in Abu Dhabi built such a platform where patients complete everything from testing to treatment within the hospital. By partnering with insurance providers, patients only pay a small portion of the cost, attracting a large number of high-end patients;
- Participating in “Patient Education and Screening Programs”: Collaborating with governments and pharmaceutical companies to conduct screening initiatives and patient education campaigns for rare diseases and cancers. Many Middle Eastern patients lack awareness of CGT therapies; screening and education help identify potential candidates while increasing treatment willingness.For example, a public hospital in Saudi Arabia participated in the government’s rare disease screening program, identifying over 200 patients suitable for CGT treatment within a year. All these patients received treatment at the hospital, boosting both its revenue and reputation.
Key Considerations:
- Develop specialized teams: Implementing CGT therapy requires dedicated physicians, nurses, and laboratory technicians. Relevant talent must be cultivated or recruited in advance.
- Establish a follow-up system: The efficacy of CGT therapies necessitates long-term monitoring and evaluation, requiring a comprehensive follow-up system, such as regular testing and patient management systems.
Type 4: Startup Technology Companies (e.g., AI interpretation, gene editing tools, cold chain logistics)
These enterprises serve as the “innovative engine” of the industrial chain—Middle Eastern governments and industrial parks are actively supporting startups by providing funding, space, and resource connections.
Collaboration Models and Layout Recommendations:
- Establish presence in industrial parks to access policy and resource support: Most Middle Eastern CGT industrial parks offer “startup incubation programs.” Participating companies gain access to free or low-cost office space, shared equipment, funding subsidies, and connections to large pharmaceutical firms within the park.For example, a startup specializing in AI-driven efficacy prediction for CGT therapies joined Abu Dhabi’s CGT Industrial Park in 2023, securing $2 million in incubation funding and partnering with Novartis to provide AI predictive services.
- Focus on niche pain points to deliver differentiated solutions: Avoid attempting to cover the entire industry chain. Instead, concentrate on specific challenges in the Middle East market, such as enhancing gene editing tool efficiency, high-temperature protection for cold chain logistics, or AI-assisted patient screening.For instance, a CGT cold chain logistics startup specializing in Middle Eastern high-temperature environments developed a specialized insulated container (maintaining low temperatures for 72 hours at 50°C), becoming a core supplier for Kuwait’s CGT logistics distribution center;
- Partner with large enterprises to achieve “technology implementation”: Startups need to collaborate with major corporations to deploy their technologies. Examples include integrating AI algorithms into equipment through partnerships with device manufacturers, or applying gene-editing tools to drug development through collaborations with pharmaceutical companies. For instance, a startup specializing in CRISPR gene-editing tool optimization partnered with a Saudi pharmaceutical company to apply its technology in developing CGT therapies for rare diseases, rapidly advancing to clinical trial stages.
Key Considerations:
- Emphasize “localized adaptation”: Startup technologies must align with Middle Eastern market demands—e.g., AI models require training on Arab populations, and cold-chain logistics must withstand high temperatures;
- Prioritize “Compliance”: Middle Eastern regulatory requirements for medtech startups are stringent. AI medical tools require HAAD/SFDA approval, while gene editing technologies necessitate ethical review—preparation must be thorough and proactive.
Finally, a core recommendation for all attendees: When establishing nucleic acid therapeutics and CGT supply chains in the Middle East, act early—the industry is still developing with relatively low competition and substantial government incentives. Once the supply chain matures, entry barriers will significantly increase.The 2026 Medlab exhibition will feature extensive participation from Middle Eastern nucleic acid therapeutics companies, CGT enterprises, and industrial park investment promotion teams. This represents an optimal opportunity to connect resources and establish collaborations—preparation is essential.

IV. Third Strategic Transformation Unveiled at 2026 Bio International Convention: Global Reshaping and Regional Focus of Industrial Chains
4. Exclusive Perspective: Medlab Middle East as a Barometer for Supply Chain Reconfiguration Linking Asia-Europe-Africa
While the first two strategic shifts represent “technology and model upgrades,” this transformation signifies a “reconfiguration of the industrial landscape.” The current IVD and precision medicine supply chains are moving beyond the outdated “Western-dominated, globally-divided” model toward a new direction of “globalized deployment + regionalized focus.” Medlab Middle East serves as the optimal barometer for observing this restructuring.
Why? Consider the Middle East’s geographic position: it connects to Europe on one side, borders Asia on another, and faces Africa to the south—a true crossroads of three continents. Previously, the Middle East served merely as the “end-consumer market” in the supply chain: importing high-end equipment from Europe, sourcing cost-effective reagents from Asia, and selling services to local and African patients.But now, the landscape is shifting. The evolution of the 2024 Medlab exhibition reveals how the Middle East is transforming from a “consumer hub” into a “hub-and-spoke” center: it must both accommodate the relocation of global industrial chains and build its own local manufacturing systems (regional focus), while leveraging its geographic advantage to become a supply chain and distribution hub connecting three continents (global restructuring).
Two core drivers underpin this shift: First, geopolitical pressures compel international buyers to diversify supply chains, moving away from reliance on single suppliers. Second, Middle Eastern governments pursue ambitious local manufacturing goals, seeking to build domestic medical technology ecosystems rather than remain import-dependent.The convergence of these factors has transformed Medlab from a mere “product trading platform” into a “strategic alignment platform” for global enterprises to position themselves within industrial chains. At the 2024 exhibition, “supply chain collaboration,” “local manufacturing,” and “regional distribution” emerged as the hottest negotiation topics, with over 60% of participating companies expressing explicit industrial chain cooperation needs.
Consider this illustrative example: At the 2022 Medlab exhibition, international companies primarily exhibited to sell products. By 2024, many international firms came to “seek partners”—such as Siemens establishing a regional manufacturing hub in Dubai requiring local distribution channels; Chinese companies entering African markets needing Middle Eastern firms as intermediaries; and African hospitals prioritizing suppliers with local inventory in the Middle East for equipment procurement.This “cross-regional, multi-link” industrial chain collaboration is ubiquitous at the exhibition.
Next, we’ll dissect the specific manifestations, opportunities, and practical recommendations of this industrial chain restructuring from two core perspectives: “supply chain resilience” and “sustainability standards.” Whether you’re a supplier, a buyer, or an entrepreneur looking to enter the market, you’ll find your niche.
4.1 Supply Chain Resilience and “Decentralization”

Amid current global geopolitical dynamics, the “decentralization” of medical supply chains has shifted from theory to practice. A prominent trend at the 2024 exhibition is international buyers actively seeking more diversified supply matrices. Dubai and Abu Dhabi are rapidly filling regional manufacturing gaps by establishing biotech free zones, attracting IVD giants—formerly reliant on imports—to establish localized production lines to mitigate potential global logistics disruptions.
4.1.1 Procurement Under Geopolitical Influence: International Buyers Pursue Diversified Supplier Strategies
The impact of geopolitics on supply chains is palpable—for instance, the Russia-Ukraine conflict has driven up energy and raw material costs in Europe, while Sino-US trade friction has restricted imports and exports of certain equipment and technologies. The Red Sea crisis has disrupted maritime shipping routes between the Middle East and Europe.These risks have fundamentally altered the procurement mindset of international buyers (especially hospitals and government procurement agencies in the Middle East): shifting from “finding the cheapest, most convenient supplier” to “building the most stable, diversified supplier portfolio.”
At the 2024 Medlab exhibition, I spoke with the head of Dubai’s government medical procurement department. He stated: “Previously, when procuring IVD equipment, we primarily focused on two metrics: price and delivery time.Now, our first priority is ‘supplier diversification’—for instance, core equipment must not be sourced from a single country; we seek at least 2-3 suppliers from different regions. Second, we assess ‘local inventory availability’—if equipment malfunctions, can we obtain parts within 72 hours instead of waiting for overseas shipments?”
To illustrate this shift in procurement strategy, I’ve compiled a comparison table highlighting the difference in Middle Eastern buyers’ past and present procurement logic:
| Procurement Decision Dimensions | Before 2020 (Old Strategy) | 2024–Present (New Strategy) | Core Reason for Change |
| Number of Suppliers | Single or a small number of suppliers (typically 2), concentrated in Europe/America or China | 3–5 suppliers covering Europe, America, Asia, and the Middle East | Avoid reliance on a single region, reduce geopolitical risks |
| Procurement Priorities | Price > Delivery time > Stability | Stability > Local Service > Price | Supply chain disruption risks outweigh cost concerns; local service enables rapid issue resolution |
| Inventory Requirements | Zero or low inventory, procure on demand | Core products must maintain 3-6 months of local inventory | Mitigate logistics disruptions to ensure supply during emergencies |
| Cooperation Model | Short-term procurement contracts (within 1 year) | Long-term strategic partnerships (3-5 years) + contingency agreements | Secure priority supply rights with premium suppliers during risk events |
| Acceptance Criteria | Focus solely on whether product specifications meet standards | Product specifications + supply chain resilience (e.g., presence of backup production facilities) + local service capabilities | Not only must the product be excellent, but the supply chain must also be reliable |
This strategic shift presents distinct opportunities and challenges for enterprises across regions—let me share real-world examples illustrating how companies are adapting:
Case Study 1: European IVD Company’s “Middle East Localized Inventory” Strategy
A renowned European IVD equipment manufacturer previously supplied the Middle East via “European production → sea freight to Dubai → distribution to customers,” with delivery times of 4-6 weeks. This model was vulnerable to disruptions like the Red Sea crisis and tariff fluctuations.In 2023, they shifted strategy: leasing a 1,000-square-meter warehouse in Dubai’s Jafza (Jebel Ali Free Zone) to pre-stock $50 million worth of core equipment and spare parts, covering demand across the Middle East and North Africa markets.
While this increased inventory costs, it yielded significant returns: During the 2024 Red Sea crisis, many sea-transport-dependent companies saw delivery times extend to 2-3 months. This company, however, leveraged its local inventory to supply customers within 72 hours. Not only did it retain existing clients, but it also captured substantial orders from competitors. In 2024, its Middle East sales grew by 40% year-over-year, with orders from local inventory accounting for over 60% of that growth.
More importantly, they secured an “Emergency Procurement Agreement” with the Dubai government. In public health emergencies (e.g., pandemics or outbreaks), the government can prioritize accessing their local inventory, while the company gains long-term procurement commitments from the government. This “risk hedging + long-term binding” model has become a core competitive advantage for European companies in the Middle East market.
Case Study 2: Chinese Companies’ “Middle East + Africa” Linked Supply Strategy
A Chinese reagent company previously faced challenges entering the African market by shipping directly from China: extended logistics cycles (3-4 weeks), high tariffs (exceeding 20% in some African countries), and slow post-sales response times. In 2024, they partnered with a Middle Eastern distributor at the Medlab exhibition, establishing a strategic collaboration:
- The Chinese company established a regional logistics hub in Dubai, stocking commonly used reagents. After African customers place orders, shipments are airfreighted from Dubai, reducing delivery times to 3-5 days.
- The Middle Eastern distributor handles channel development and after-sales service in Africa, while the Chinese company provides products and technical support;
- To address tariffs, they leverage free trade agreements between the Middle East and select African nations. Reagents are first exported to Dubai (enjoying zero tariffs) before being shipped to Africa, reducing tariffs by 10-15%.
Following this strategy, the Chinese company rapidly expanded its market share in Africa—achieving over $20 million in sales in the second half of 2024. Short delivery times and prompt after-sales service have also driven high customer satisfaction. Crucially, using the Middle East as a “stepping stone” bypassed direct market entry barriers in Africa, reducing channel and logistics risks while lowering market development hazards.
Case Study 3: Middle Eastern Local Enterprise’s “Diversified Supplier Integration” Strategy
A major Middle Eastern healthcare group, operating over 50 hospitals and laboratories, previously sourced core equipment primarily from Europe. After 2022, they initiated a “supplier diversification” plan:
- Core Equipment: European brands (40%) + Chinese brands (30%) + Local brands (30%) — e.g., European sequencing instruments for high-end facilities, Chinese biochemical analyzers for routine testing, and local POCT devices for primary clinics;
- Supplies and Reagents: At least two suppliers from different regions per category. For instance, European reagents for high-end hospitals, Chinese reagents for routine testing, and local reagents for primary care clinics;
- Establish a “Supplier Evaluation System”: Quarterly assessments of suppliers’ delivery reliability, after-sales response speed, and price volatility. Eliminate underperforming suppliers and add new high-quality ones.
After implementing this plan, the healthcare group significantly reduced supply chain risks: In 2023, when a European brand delayed deliveries due to chip shortages, they immediately switched to backup equipment from a Chinese brand, ensuring no disruption to hospital operations. Furthermore, competition among suppliers drove average procurement costs down by 8%, while after-sales response times shortened from 48 hours to 24 hours.
For attendees, this shift in procurement strategy presents three core opportunities:
- If you are an international supplier: Establish “local inventory + local service” capabilities in the Middle East. Even a small logistics center can significantly boost competitiveness—Middle Eastern buyers now prioritize “supply reliability during emergencies.”
- If you are a Chinese supplier: Consider the Middle East as a “stepping stone” to enter the African market. Partner with local distributors to address logistics and channel issues—the African market has enormous demand, but direct entry barriers are high, making the Middle East the optimal transit point.
- If you are a local supplier: This presents a prime opportunity to leapfrog ahead. Middle Eastern buyers are now actively supporting local enterprises. As long as your product quality meets standards and you leverage local service advantages, securing government and hospital contracts becomes highly achievable.
Of course, challenges exist: establishing local inventory requires capital investment, finding local partners demands time for collaboration, and navigating varying tariffs and trade policies across countries necessitates specialized knowledge. Yet these challenges are surmountable—for instance, many Middle Eastern free zones (such as JAFZA and Abu Dhabi’s Khalifa Industrial Zone) offer “inventory financing” services to alleviate funding pressures.Medlab itself serves as an optimal platform for finding partners, with numerous local distributors actively seeking international suppliers at the exhibition.
4.1.2 Middle East’s Local Manufacturing Ambition: Dubai/Abu Dhabi Attracts IVD Manufacturers to Establish Regional Hubs
While “supply chain diversification” is driven by external demand, “local manufacturing” represents an active strategy by Middle Eastern governments. They aim to move beyond being merely the “end of the global industrial chain” and instead build their own “medical technology manufacturing hubs.” This vision seeks to transform the region from a consumer of medical products into a producer and exporter of high-value-added IVD equipment and precision medicine products.
This ambition is most directly reflected in the series of “nest-building” policies launched by Dubai and Abu Dhabi—covering everything from tax exemptions and expedited approvals to infrastructure support and market access, addressing nearly all requirements for business establishment. I have compiled the core investment promotion policies of these two cities for your reference:
| Policy Dimensions | Dubai (JAFZA/Medical Free Zone) | Abu Dhabi (Khalifa Industrial Zone/CGT Industrial Park) | Core Attraction for Enterprises |
| Tax Incentives | 15-year tax exemption (full exemption from corporate income tax, VAT, and customs duties), renewable for an additional 15 years upon expiration | 20-year tax exemption, plus an additional 5-year R&D subsidy (covering up to 50% of R&D costs) for CGT and IVD high-end manufacturing enterprises | Significantly reduced operating costs, particularly advantageous for capital-intensive manufacturing enterprises |
| Approval Speed | Business license approved within 3-5 working days; medical device registration processing time reduced by 50% (through a green channel established in collaboration with HAAD) | Manufacturing license approved within 7 working days; CGT product registration approval time reduced by 60% compared to standard procedures (mutual recognition agreements with FDA/EMA) | Rapid production ramp-up avoids prolonged approval delays |
| Infrastructure | Standardized GMP facilities (customizable upon request), shared wastewater treatment, cold chain storage, and quality testing center | Integrated “facility + lab + logistics center” solutions with dedicated CGT production infrastructure (e.g., bioreactors, cold chain logistics) within the park | Eliminate infrastructure construction costs, reducing initial investment |
| Financial Support | For enterprises with investments exceeding $10 million, provide up to 20% fixed asset investment subsidies | Establishment of a $2 billion manufacturing fund offering equity financing to high-quality enterprises (holding no more than 20% equity without operational interference) | Alleviates capital pressure, particularly suitable for manufacturing startups |
| Market Access | Signing procurement framework agreements with the Dubai government and local hospitals to prioritize procurement orders for resident enterprises | Collaborate with healthcare institutions in GCC countries to enable rapid inclusion of resident enterprises’ products into the healthcare reimbursement lists of six countries | Resolve market distribution challenges and accelerate commercialization |
| Talent Support | Offer talent recruitment subsidies (including three years of tax-exempt salaries for high-end technical personnel) and partner with local universities for targeted technical workforce training | Establish a “Manufacturing Talent Training Center” to provide free technical worker training for enterprises; high-end talent may receive housing subsidies | Address local talent shortages and reduce recruitment costs |
These policies are not empty promises but tangible initiatives with concrete outcomes—at the 2024 Medlab Exhibition, investment promotion teams from Dubai and Abu Dhabi showcased their latest achievements:
Case Study 1: Siemens’ Regional Manufacturing and Distribution Center in Dubai
In 2023, Siemens invested $200 million to establish a regional manufacturing and distribution center for IVD equipment in Dubai’s JAFZA, marking its first manufacturing base in the Middle East. This facility primarily produces high-demand equipment like routine biochemical analyzers and immunoassay analyzers while serving as a distribution hub for European and Asian products to the Middle East, Africa, and Central Asia.
The core reasons for choosing Dubai were its policy and geographical advantages: On one hand, a 15-year tax exemption policy significantly reduced operational costs; on the other, shipping from Dubai to Africa and Central Asia cut logistics time by half compared to shipments from Europe, enabling better service to regional markets.By 2024, the center had commenced production with an annual output of 5,000 units, 60% of which supply the Middle East locally while 40% are exported to Africa and Central Asia. Sales are projected to exceed $300 million by 2025.
More importantly, this center has spurred the clustering of upstream and downstream industrial chains. Currently, three Chinese reagent manufacturers and two European parts suppliers have followed Siemens into JAFZA, forming a small industrial cluster encompassing “equipment manufacturing + reagent supply + parts maintenance.” This model of “flagship enterprise leadership + industrial chain clustering” precisely aligns with Dubai’s strategic objectives.
Case Study 2: Chinese Enterprise’s “CGT Reagent Localization Project” in Abu Dhabi
A Chinese company specializing in CGT reagents connected with Abu Dhabi’s investment promotion team at the 2024 Medlab exhibition and decided to invest $50 million to establish a localized production base in Abu Dhabi’s CGT Industrial Park. This facility will primarily manufacture core CGT consumables such as gene editing reagents and cell culture reagents, supplying CGT enterprises across the Middle East and Europe.
Beyond the 20-year tax exemption policy, the company was drawn by Abu Dhabi’s R&D subsidies and market access support: enterprises can receive 40% subsidies on R&D costs, and products can be rapidly included in the GCC countries’ national health insurance reimbursement lists.More importantly, the CGT Industrial Park already hosts international giants like Novartis and Bluebird Bio. By establishing operations there, the company can directly integrate into these firms’ supply chains as reagent suppliers—a far faster route than independently developing the market.
Currently under construction, this production base is slated for commissioning in 2025, with projected annual sales reaching $150 million. Furthermore, the company plans to leverage Abu Dhabi’s policy advantages to pursue FDA and EMA certifications, enabling global market access—transforming the Middle Eastern manufacturing base into a springboard for worldwide expansion.
Case Study 3: Middle Eastern Local Enterprise’s “IVD Equipment Assembly and Upgrading Project”
Bayanat, a local Middle Eastern enterprise previously focused on medical data services, transitioned into IVD manufacturing in 2023. They established an equipment assembly and upgrade base in Dubai’s Healthcare Free Zone. Their model is highly flexible: sourcing core components from China, assembling and debugging them in Dubai, and performing localized upgrades (such as adapting to Middle Eastern voltage standards and adding Arabic interfaces), then selling the products under a local brand.
This model offers “low costs and rapid response”: sourcing core components from China reduces costs by 30% compared to Europe. Post-local assembly, they swiftly address customized client needs—such as hospitals requiring specific testing functions—completing upgrades within 1-2 weeks. By 2024, their products had entered over 10 public hospitals in Dubai and Saudi Arabia, achieving sales exceeding $80 million. As a local brand, they also secured preferential government procurement treatment.
For attendees, the Middle East’s local manufacturing wave presents a “low-barrier, high-return” entry opportunity, though different enterprise types require distinct approaches:
- If you are an international giant: Establish a regional manufacturing hub in Dubai or Abu Dhabi to leverage policy advantages for cost reduction while serving the Middle East, Africa, and Central Asia markets—a crucial step in building a global supply chain.
- For small-to-medium equipment/reagent companies: Adopt an “import core components + local assembly” model to reduce initial investment while leveraging local brand recognition and policy support for rapid market penetration;
- If you are a supply chain enterprise (e.g., logistics, parts, quality inspection): Follow leading companies into industrial parks to provide supporting services—demand generated by industrial cluster aggregation offers far greater stability than independent market expansion;
- If you are an investor: Focus on Middle Eastern manufacturing funds or directly invest in promising local manufacturers—the region’s medical manufacturing sector is experiencing rapid growth with substantial investment return potential.
However, establishing local manufacturing requires attention to several key points: First, select the right industrial park, as policies vary significantly between parks (e.g., Dubai’s JAFZA suits distribution-oriented manufacturing, while Abu Dhabi’s CGT Industrial Park caters to high-end manufacturing). Second, prioritize localization adaptation—ensure product voltage, language, and compliance standards meet Middle Eastern requirements. Third, secure local partnerships, particularly for distribution channels and government relations, which can save considerable time and effort.
4.2 Sustainability Emerges as the New Quality Standard
Historically, product or laboratory quality was evaluated primarily by “accuracy,” “efficiency,” and “price.” Today, however, “sustainability” (commonly referred to as “environmental friendliness”) has emerged as a core quality standard—particularly in the Middle East. As governments prioritize sustainable development, environmental certifications have shifted from “bonus points” to “mandatory requirements.” Without relevant certifications, companies may not even qualify for government tenders.
This shift stems from Middle Eastern governments’ “green transition” strategies—such as the UAE’s “Net Zero Emissions Strategy 2050” and Saudi Arabia’s “Green Saudi Initiative”—which prioritize sustainability in the healthcare sector.For laboratories, “green labs” not only meet policy requirements but also reduce long-term operational costs (e.g., energy savings, lower waste disposal fees), achieving a win-win of environmental protection and cost savings. For enterprises, environmental certifications serve as a “stepping stone” to enter the Middle East market while enhancing brand image.
4.2.1 The ROI of Green Labs: How Energy Efficiency and Waste Management Reduce Long-Term Operating Costs
Many assume “going green costs a fortune,” but the opposite is true—the core of green labs lies in “resource efficiency.” By optimizing energy consumption, minimizing waste generation, and recycling resources, they significantly reduce long-term operational expenses. Let’s break down the numbers and examine real-world impact through case studies:
First, let’s examine the operational cost differences between traditional and green laboratories. A comparison table provides clarity:
| Cost Item | Traditional Lab (1,000 sq m) | Green Lab (1,000 sq m) | Annual Cost Savings | Payback Period |
| Electricity Consumption (Including Equipment, Air Conditioning, Lighting) | Annual electricity cost: approximately $150,000 (average $1.25/kWh) | Annual electricity cost: approx. $80,000 (energy-efficient equipment + smart control system, 47% power savings) | $70,000 | 2-3 years |
| Water consumption (including experimental water and cleaning water) | Annual water cost: approximately $30,000 (average $5/cubic meter) | Annual water bill: approximately $12,000 (water recycling system, 60% water savings) | $18,000 | 1.5-2 years |
| Waste disposal fees (including medical waste, chemical waste) | Annual processing fee: approximately $60,000 (based on 10 tons/month) | Annual processing fee: approx. $24,000 (reduced waste generation + sorting/recycling, 60% emissions reduction) | $36,000 | 1-2 years |
| Consumables cost (including reagents, disposable supplies) | Annual consumables cost: approximately $500,000 | Annual consumables cost: approx. $425,000 (consumables recycling + precision procurement, saving 15%) | $75,000 | 1 year |
| Other costs (e.g., maintenance fees, compliance penalties) | Approximately $50,000 per year (potential environmental fines) | Approx. $30,000/year (lower maintenance costs for green equipment, no environmental fines) | $20,000 | – |
| Total annual operating costs | $790,000 | $569,000 | $221,000 | Average 2 years |
| Initial renovation/construction additional investment | – | Approx. $450,000 (energy-efficient equipment, water recirculation systems, waste treatment facilities) | – | 2 years |
This table shows that the initial additional investment for a green lab is approximately $450,000. However, it saves $221,000 in annual operating costs, recouping the investment in just 2 years on average. After that, it nets over $200,000 in savings each year—this is the ROI (Return on Investment) of a green lab, making it highly cost-effective in the long run.
Below are two real-world examples of green laboratories in the Middle East, demonstrating how they achieve both environmental sustainability and cost savings:
Case Study 1: Dubai Private Hospital’s “Smart Energy-Efficient Green Lab”
This hospital’s 1,200-square-meter laboratory underwent a green retrofit in 2023, focusing on three key areas:
- Replacing energy-efficient equipment: Traditional sequencing instruments and biochemical analyzers were swapped for energy-saving models, reducing power consumption by 40%. A smart lighting system was also installed, activating lights when occupied and deactivating them when unoccupied, while automatically lowering air conditioning temperatures during unmanned periods.
- Establishing a water recycling system: Installing greywater recovery equipment to collect and treat post-experiment clean water and air conditioning condensate for laboratory cleaning and landscaping irrigation, saving 6,000 cubic meters of water annually;
- Waste Segregation and Recycling: Established a comprehensive waste classification system—medical waste (e.g., used test tubes, swabs) is separately collected for professional disposal; chemical waste (e.g., spent reagents, solvents) undergoes distillation recovery with partial reuse; single-use consumables (e.g., plastic centrifuge tubes) utilize biodegradable materials for post-use recycling and decomposition.
The total renovation investment was $500,000, yielding particularly impressive results:
- Annual electricity costs decreased from $180,000 to $95,000, saving $85,000;
- Annual water costs decreased from $36,000 to $14,000, saving $22,000;
- Annual waste disposal costs decreased from $72,000 to $28,000, saving $44,000;
- Annual consumables costs decreased from $600,000 to $510,000, saving $90,000;
- Total annual savings: $241,000, with an investment payback period of less than two years.
More importantly, by meeting green standards, the laboratory earned LEED Gold certification. This not only gave it an edge in government tenders but also attracted many environmentally conscious high-end patients, significantly enhancing the hospital’s brand image.
Case Study 2: Abu Dhabi Public Health Laboratory’s “Waste-to-Resource Green Laboratory”
This laboratory is a flagship green demonstration project developed by the Abu Dhabi government, with its core highlight being “waste-to-resource conversion”—turning former “waste” into “resources”:
- Chemical Waste Recycling: Spent reagents and solvents are distilled and purified using specialized equipment. Once purity standards are met, they are reused in routine experiments—recovering approximately 2 tons of chemical reagents annually and saving about $80,000 in procurement costs.
- Medical Waste Neutralization: Used test tubes, petri dishes, and other medical waste undergo high-temperature sterilization and pulverization to produce recycled plastic pellets. These pellets are sold to local plastic manufacturers for non-medical applications—generating approximately 3 tons of recycled plastic annually and yielding additional revenue of about $15,000 USD;
- Energy self-sufficiency: Solar panels installed on the laboratory roof generate approximately 120,000 kWh of electricity annually, meeting 40% of the laboratory’s power needs and saving about $50,000 in electricity costs each year.
This lab achieved “turning waste into resources” without significant additional renovation investment, primarily through process optimization and introducing resource recovery equipment. By 2024, its operational costs had decreased by 30% compared to pre-renovation levels. As a government demonstration project, it also received a $200,000 green subsidy. More importantly, its model has been replicated across 10 other public laboratories in Abu Dhabi, driving a regional green transformation of laboratory operations.
Some may ask: “Can our small-scale lab achieve green transformation too?” Absolutely—green transformation isn’t exclusive to large facilities. Small and medium-sized enterprises (SMEs) and grassroots labs can start with low-cost initiatives:
- For instance, switching to LED energy-saving bulbs and installing smart outlets (to prevent standby power consumption) requires an investment of just a few hundred dollars and can save 10-15% on annual electricity bills.
- Procuring reusable lab consumables (e.g., glass centrifuge tubes, stainless steel tweezers) may have higher upfront costs than disposables, but long-term use can reduce consumable expenses by over 30%.
- Establishing a simple waste sorting system to separate recyclable plastics and glass for sale to recycling companies reduces disposal fees while generating modest revenue.
These small measures may seem insignificant, but over time they significantly reduce operating costs and lay the groundwork for future environmental certifications—as Middle Eastern environmental policies tighten, early transition brings early benefits.
4.2.2 Value for Stakeholders: Environmental Certification as a Mandatory Requirement for Multinational Hospitals and Government Tenders
If the ROI of green labs represents “internal motivation,” environmental certifications constitute “external pressure.” Today, multinational hospitals and government tenders in the Middle East mandate environmental certifications as prerequisites. Without them, even the most superior or cost-effective products are ineligible for participation.
Currently, the Middle East market recognizes three primary types of environmental certifications. I have compiled a detailed certification guide for you, covering certification types, applicable scenarios, application difficulty, and core value:
| Certification Type | Core Standards | Applicable Scenarios | Application Difficulty | Application Cycle | Core Value in Middle East Market |
| LEED Certification (Leadership in Energy and Environmental Design) | Evaluates building sustainability across multiple dimensions including energy, water resources, waste management, and indoor environmental quality | New construction or renovation of laboratories and hospital buildings | ★★★☆☆ | 3-6 months | Essential requirement for government tenders and multinational hospital procurement; enhances brand image and qualifies for policy subsidies |
| ISO 14001 Environmental Management System Certification | Requires enterprises to establish a comprehensive environmental management system to control environmental impacts during production and operations | Equipment manufacturers, reagent producers, laboratory operators | ★★★☆☆ | 2-4 months | A “stepping stone” for entering the Middle East market; a fundamental requirement for multinational corporate partnerships; certain government projects may offer price incentives |
| TÜV Rheinland Green Product Certification | Evaluates the environmental impact of IVD devices, reagents, and related products throughout their entire lifecycle (e.g., energy consumption during production, product recyclability) | IVD devices, reagents, consumables, and related products | ★★★★☆ | 4-8 months | Differentiated competitive advantage in premium markets; secures priority procurement rights with multinational hospitals; enables 10-15% product premium potential |
Consider this cautionary tale of a missed order due to certification to underscore its critical importance:
In 2024, a Chinese IVD equipment manufacturer participated in a Saudi government medical equipment tender. Their product specifications and pricing outperformed competitors, yet they ultimately lost the bid—simply because rivals held ISO 14001 and LEED certifications, while they lacked any environmental certifications, failing to meet mandatory tender requirements. This $20 million tender was lost due to missing two certifications.
Meanwhile, another Chinese reagent company proactively obtained ISO 14001 certification. At the 2024 Medlab exhibition, this certification alone secured them cooperation agreements with two multinational hospitals in Dubai. The hospital procurement managers explicitly stated they only partner with environmentally certified companies, citing corporate sustainability policies as the requirement.
Therefore, for attendees, applying for environmental certifications is not an “option” but a “mandatory requirement”—especially for those targeting the Middle East’s government and high-end healthcare markets, where certification is an unavoidable threshold. Below is a “Practical Guide to Applying for Environmental Certifications” to help you avoid unnecessary detours:
Step 1: Select the appropriate certification based on your circumstances
- If you operate a laboratory: Prioritize LEED certification (for buildings) and ISO 14001 certification (for operations)—these are fundamental requirements for government tenders and hospital partnerships.
- If you are an equipment/reagent manufacturer: Prioritize ISO 14001 certification (for enterprises) and TÜV Rheinland Green Product Certification (for products)—ISO 14001 is the foundation for market entry, while TÜV Rheinland can help you access premium markets;
- If you are an SME with limited budget: Start with ISO 14001 certification (lower application cost, faster return on investment), then pursue other certifications as your business grows.
Step 2: Prepare for certification in advance to increase pass rates
- Establish an environmental management system: Develop policies for energy/water conservation and waste management, and maintain daily environmental data records (e.g., energy consumption, waste generation) — core requirements for ISO 14001 certification.
- Optimize products and operational processes: Equipment manufacturers can refine production techniques to reduce energy consumption and waste generation; laboratories can upgrade to energy-efficient equipment and implement waste sorting systems—these improvements boost pass rates for LEED and TÜV certifications;
- Partner with local certification bodies: The Middle East hosts numerous authoritative certification bodies (e.g., UAE’s ESMA, Saudi Arabia’s SASO). Collaborating with local agencies not only ensures familiarity with regional regulations but also accelerates the certification process—avoiding potential failures due to standard mismatches when engaging international bodies.
Step 3: Leverage certification advantages to expand markets
- Prominently display certification results: Feature certification logos at trade show booths, in product manuals, and on website homepages for immediate visibility to buyers.
- Leverage government green initiatives: Middle Eastern governments fund numerous green healthcare projects (e.g., green hospital construction, green lab retrofits). Proactively engage with these programs, using certifications as a bargaining chip for collaboration.
- Build a “Green Brand” Image: During promotions, emphasize the sustainability of products and services. Examples include: “Our equipment consumes 40% less energy than industry averages” or “Our reagents contain 60% recyclable components.” This approach attracts environmentally conscious clients.
Finally, a timeline recommendation: Environmental certification typically takes 2-8 months to obtain. We advise completing certification before the 2026 Medlab exhibition. This allows you to present your credentials directly during exhibition negotiations, boosting partnership success rates. Additionally, many Middle Eastern governments offer subsidies to certified companies. Apply for these subsidies concurrently with certification to reduce costs.
4.2.3 Summary
This “global restructuring + regional focus” of the industrial chain presents a “reshuffling opportunity” for all participants: Seizing the trend toward supply chain diversification by establishing local inventory or manufacturing bases in the Middle East enables mitigation of geopolitical risks and access to three major continental markets. Completing green transformation early and securing environmental certifications grants a competitive edge in government tenders and high-end markets.
Medlab Middle East 2026 will serve as the pivotal convergence point for this supply chain restructuring—gathering global suppliers, buyers, and partners to negotiate supply chain collaborations, local manufacturing projects, and green certification partnerships. For attendees, this event is less about “attending an exhibition” and more about “charting your supply chain strategy for the next five years.”

V. Practical Action Checklist for 2026 Bio International Convention Attendees and Industry Observers
5. Exclusive Fresh Perspective: Translating High-Level Trends into Immediately Actionable Business Strategies
After discussing industry transformation, technological trends, and industrial chain opportunities, some may ask: “I understand the concepts, but how do I actually implement them?” This chapter addresses that core question—breaking down high-level trends into concrete actions you can execute around the 2026 Medlab exhibition.
Whether you’re an enterprise decision-maker, laboratory director, startup founder, or industry observer, the action list follows the same core logic: focus on the essentials, turn “trends” into “specific tasks,” and transform “opportunities” into “tangible outcomes.“ After all, trade shows are like an industry entrance exam. Only through advance preparation and targeted efforts can you secure the resources and orders you seek. If you merely skim the surface, taking in the spectacle before moving on, you’ll miss the prime opportunity to recalibrate your strategy.
To translate these macro trends into concrete business decisions, we have distilled strategic action goals for industry observers in various roles around the 2026 exhibition. These recommendations aim to help you pinpoint the most certain growth opportunities amid intense market volatility.
5.1 Three Core Action Goals for the Period Around the 2026 Exhibition
These three objectives serve as the “core missions” before and after the exhibition, covering three critical dimensions: “Talent, Partners, and Risk.” Talent forms the foundation for execution, partners drive expansion, and risk mitigation ensures steady development. We recommend breaking down these objectives into specific responsibilities and timelines to ensure closed-loop implementation before and after the exhibition.
5.1.1 Goal One: Address Talent Gaps—Assess team capabilities in AI/bioinformatics and develop recruitment/internal training plans
As repeatedly emphasized, one core challenge in the Middle East market is the shortage of AI/bioinformatics talent. This deficiency is critical across automation 2.0, multi-omics analysis, and the CGT supply chain. Without addressing this gap now, securing orders or partners will prove futile—this is why many companies stumble in the Middle East.
Therefore, the first actionable goal is to complete a “talent capability assessment” before the 2026 exhibition, connect with talent resources during the event, and implement recruitment/internal training plans afterward.
Step 1: Conduct a “Talent Capability Matrix Assessment” — Identify Your Shortcomings
Many companies remain unaware of their talent gaps, either hiring indiscriminately or assuming “no suitable candidates exist.” A “competency matrix” offers a clear and efficient solution for rapid assessment:
| Core Competency Modules | Competency Requirements (aligned with the trends mentioned earlier) | Current Team Level (1-5 points, 1 = completely unskilled, 5 = proficient) | Gap Severity (5 – Current Score) | Priority (High/Medium/Low) |
| AI Tool Application | Ability to operate AI data analysis platforms (e.g., Illumina BaseSpace) and interpret AI analysis reports | |||
| Bioinformatics analysis | Capable of processing NGS raw data, interpreting multi-omics data, and integrating clinical reports | |||
| Automated Equipment Operation | Proficient in operating digital twin systems and automated pipelines, troubleshooting common malfunctions | |||
| CDx Collaboration Capabilities | Understands CDx-drug collaboration logic and is familiar with CDx registration processes in the Middle East | |||
| CGT Industry Chain Knowledge | Comprehends CGT manufacturing processes, clinical trial requirements, and cold chain logistics standards | |||
| Green Laboratory Operations | Proficient in operating energy-efficient equipment, waste sorting and recycling, and applying for environmental certifications |
Scoring Guidelines:
- 1-5 point assessments should be objective. For example, “Can operate AI platforms but cannot customize algorithms” would receive a 3.
- Gap Level = 5 – Current Score; higher scores indicate larger gaps
- Priority: Mark “High” for skills strongly relevant to core business (e.g., bioinformatics analysis must be high priority for multi-omics service providers); mark “Medium” for skills needed within 1-2 years; mark “Low” for skills not currently required.
Example: If your company sells IVD equipment and focuses on promoting Automation 2.0 devices, “Automated Equipment Operation” and “AI Tool Application” are high priority. If you supply CGT reagents, “CGT Supply Chain Knowledge” and “Bioinformatics Analysis” are high priority.
Step 2: Select a “Hiring + Internal Training” Combination Based on Gaps
After assessing gaps, avoid trying to “bite off more than you can chew.” Prioritize gaps and adopt a hybrid approach: “external hiring for core competencies, internal training for foundational skills.” After all, recruiting high-end talent in the Middle East is challenging, while internal training rapidly builds foundational capabilities at a better cost-effectiveness ratio.
| Gap Types | Solutions | Implementation Steps | Timeline (Example: 2026 Exhibition) | Case References |
| High-priority core talent (e.g., bioinformatics specialists, AI algorithm engineers) | External recruitment + local partnerships | 1. 3 months before the exhibition: Post job openings on local Middle Eastern recruitment platforms (e.g., Bayt, Naukrigulf) and industry communities;<br>2. During the exhibition: Participate in the “Talent Matching Session” to connect with talent resources from universities and research institutions;<br>3. One month after the exhibition: Complete the onboarding of 1-2 core talents;<br>4. Long-term: Collaborate with local Middle Eastern universities (e.g., Mohamed bin Zayed University) on “targeted training programs” to secure graduates in advance | Recruitment initiated 3 months prior to the exhibition, with onboarding completed within 1 month post-event | A Chinese AI healthcare company participated in the Talent Matching Session during the 2024 exhibition, connecting with 2 local Dubai bioinformatics experts. After onboarding, they rapidly completed the localization adaptation of a multi-omics data interpretation platform, securing 2 hospital orders within 3 months. |
| Mid-priority foundational talent (e.g., automated equipment operators, AI platform operators) | Internal training + external empowerment | 1. Two months before the exhibition: Identify 2-3 employees with strong learning capabilities within the team;<br>2. During the exhibition: Arrange for employees to attend the exhibition’s “technical training workshops” to learn AI platform and automated equipment operation;<br>3. Two months after the exhibition: Collaborate with equipment suppliers to conduct internal training (e.g., Siemens automated equipment training, Illumina AI platform training);<br>4. One month after training: Conduct assessments to ensure employees can operate independently | Select employees 2 months before the exhibition; complete training and assessments within 3 months post-exhibition | A grassroots laboratory in Dubai arranged for 3 nurses to attend POCT sequencing equipment training at the 2024 exhibition. Post-exhibition, they partnered with Oxford Nanopore for internal training. Within 3 months, nurses could independently perform rapid infectious disease testing, boosting the lab’s testing capacity by 40%. |
| Low-priority reserve talent (e.g., Green Lab Operations Specialist) | Online courses + part-time consultants | 1. Within 3 months post-exhibition: Assign one employee to complete online courses (e.g., LEED green building certification);<br>2. Long-term: Engage external part-time consultants (e.g., experts from environmental certification bodies) to provide guidance as needed | Initiate learning within 3 months post-exhibition; maintain ongoing collaboration | A Saudi Arabian SME hospital scheduled administrative staff to take online green lab courses in 2024 while hiring an environmental consultant to guide waste sorting. Six months later, it successfully obtained ISO 14001 certification and secured government green healthcare subsidies. |
Key Reminder: Middle East Recruitment/Internal Training Pitfall Guide
- Prioritize “local experience” in hiring: For instance, when recruiting bioinformatics specialists, prioritize candidates with experience interpreting Middle Eastern population data and familiarity with local compliance requirements to avoid unnecessary detours.
- In-house training must “align with practical needs”: Avoid generic AI courses. Focus on training for specific platforms your team uses (e.g., BaseSpace, Watson) to ensure immediate application after completion.
- Leverage “Government Subsidies” to Reduce Costs: Many Middle Eastern governments offer subsidies for corporate talent development and high-level talent recruitment (e.g., Dubai’s “Talent Development Fund”). Proactively apply for these programs, which can cover 30%-50% of costs.
5.1.2 Objective Two: Strategic Partner Screening—Compile a list of the top five most promising technologies/companies for the next five years
Medlab 2026 is not merely a “product trade show” but a “strategic partnership matchmaking event”—every company and technology provider you encounter could become a core partner in your next five years. However, with the exhibition’s crowded and diverse environment, lacking clear screening criteria can easily lead to being overwhelmed by sales pitches, resulting in “many discussions but no concrete outcomes.”
Therefore, the second action goal is to define selection criteria before the exhibition, conduct targeted matchmaking during the event, and identify five most promising partners post-exhibition to establish long-term collaborations.
Step 1: Define “Partner Screening Criteria” — Avoid Blind Matchmaking
Different attendee types have varying criteria, but all core standards revolve around three dimensions: “technical compatibility, resource complementarity, and long-term mutual benefit.” Below are tailored screening templates for different roles, ready for your modification:
| Participant Role | Core Selection Dimensions | Specific Criteria | Red Flags (Immediately Reject in These Cases) |
| Corporate Decision-Makers (Equipment/Reagent Suppliers) | 1. Complementary market coverage (e.g., can help you enter the African market);<br>2. Technological synergy (e.g., can address gaps in your AI or CGT capabilities);<br>3. Resource endorsement (e.g., government partnerships, high-profile client cases) | 1. Established distribution channels or local inventory in the Middle East;<br>2. Technology aligns with the three major transformation trends (e.g., Automation 2.0, Multi-omics, Green Sustainability);<br>3. 2-3 successful case studies in the Middle East;<br>4. Willingness to sign a long-term strategic cooperation agreement (3-5 years) | 1. Lack of local regulatory compliance (e.g., HAAD/SFDA registration);<br>2. Outdated technology (e.g., traditional automation equipment without AI capabilities);<br>3. Focus solely on short-term gains without commitment to long-term partnership |
| Laboratory Director | 1. Products/services address core pain points (e.g., shorten TAT, reduce costs);<br>2. Strong local service capabilities (e.g., rapid after-sales response, local technical support);<br>3. High compliance (e.g., data security, environmental certifications) | 1. Product specifications meet clinical requirements (e.g., sequencing accuracy ≥99.5%, TAT ≤48 hours);<br>2. After-sales response time ≤24 hours with local service team;<br>3. Possesses relevant certifications (e.g., LEED, ISO 14001);<br>4. Offers customized solutions (e.g., integration with existing lab systems) | 1. Product lacks local registration certification, preventing hospital approval;<br>2. After-sales support requires overseas team dispatch with response times exceeding 72 hours;<br>3. Data cannot integrate with local health platforms, posing high compliance risks |
| Startup Founder | 1. Resource empowerment (e.g., providing funding, channels, or customer resources);<br>2. Technical complementarity (e.g., enhancing product implementation capabilities);<br>3. Shared vision (e.g., valuing long-term growth over short-term monetization) | 1. Possesses local Middle Eastern resources (e.g., government partnerships, industrial park access);<br>2. Can address core weaknesses (e.g., distribution channels, regulatory compliance);<br>3. Willing to provide funding/resources without interfering in product development;<br>4. Has proven track record of incubating successful startups | 1. Seeks only to acquire your technology without long-term commitment;<br>2. Lacks local resources to facilitate market entry;<br>3. Demands short-term profitability, which contradicts startup development cycles |
Step 2: “Precision Matchmaking” During the Exhibition—Efficient Partner Screening
Exhibition time is limited (typically 3-4 days). Blindly browsing booths wastes time. Prepare a “matching list” in advance, prioritize companies, and schedule targeted meetings:
- One month before the exhibition: Visit Medlab’s official website to review the list of participating companies. Based on your selection criteria, identify 20-30 target companies. Schedule meetings in advance via email or the official website (mention “strategic cooperation discussion” to increase response rates).
- During the exhibition: Schedule 4-5 targeted meetings daily, each lasting 30 minutes. Focus on three key questions: “What are your core resources in the Middle East?” “What specific challenges can you help us solve?” “What long-term cooperation models are you open to?” Simultaneously, observe their product/technology demonstrations on-site to verify alignment with promotional claims.
- Daily Wrap-Up: Spend 1 hour reviewing each day’s meetings, score them on a 10-point scale, and select 10 candidate partners. Note their core strengths and potential collaboration areas.
Step 3: Post-Exhibition “Lock in Top Five Potential Partners” — Create List and Follow Up
Within one week after the exhibition, based on the match results and scores, finalize a list of 5 partners deemed “most promising for the next five years.” Clearly define cooperation priorities and next steps:
| Partner Name | Industry | Core Strengths (Tailored to Your Needs) | Collaboration Areas | Next Steps (Timeline) | Responsible Party |
| Example: A Dubai-based distribution company | Medical Distribution | Distribution channels covering 15 countries across the Middle East and Africa, with local inventory | Leverage its channels to enter the African market and jointly establish regional logistics centers | Within 2 weeks post-exhibition: Sign framework cooperation agreement;<br>Within 1 month post-exhibition: Finalize first batch of cooperative products | Mr. Zhang |
| Example: An AI healthcare company | Multi-omics AI interpretation | Possesses an Arab population database with 92% AI interpretation accuracy | Collaborative development of localized multi-omics interpretation platform | Within 3 weeks post-exhibition: Complete technical integration demonstration;<br>Within 2 months post-exhibition: Initiate joint R&D | Manager Li |
| … | … | … | … | … | … |
Case Study: In 2024, a Chinese POCT equipment manufacturer pre-selected 25 target partners. During the exhibition, they held discussions with 18 of them and ultimately secured 5 partners:1 Dubai-based distributor (covering Middle East + Africa channels), 1 local after-sales service provider (handling on-site technical support), 1 AI company (specializing in data interpretation), 1 environmental certification agency (managing ISO 14001 certification), and 1 industrial park (facilitating future local assembly). Within three months post-exhibition, they rapidly entered the Saudi and Nigerian markets through these partners, securing $30 million in orders—demonstrating the power of precise partner selection.
5.1.3 Objective Three: Market Risk Hedging—Review Supply Chain/Distribution Network to Mitigate Logistics and Cost Pressures
As discussed earlier, geopolitical tensions, logistics disruptions, and rising costs are primary risks in the Middle East market. These risks aren’t a matter of “if” but “when.” Therefore, the third action goal is to conduct a “risk assessment” of the supply chain/distribution network before and after the exhibition and implement hedging solutions to ensure business continuity regardless of circumstances.
Step 1: Create a “Risk Assessment Checklist” — Identify Potential Vulnerabilities
Use the checklist below to systematically assess your supply chain/distribution network. Mark high-risk areas with a “✓” for prioritized attention:
| Risk Type | Checklist Items | High-Risk Points (Check “√”) | Potential Impact |
| Supply Chain Risk | 1. Are core suppliers concentrated in 1-2 countries/regions?<br>2. Are critical components/reagents dependent on a single supplier?<br>3. Is there no local inventory in the Middle East, relying entirely on international logistics?<br>4. Does the logistics route solely depend on the Red Sea-Suez Canal shipping lane? | Stockouts, extended delivery times, increased costs | |
| Distribution Network Risks | 1. Are distribution channels concentrated in 1-2 core cities (e.g., Dubai, Riyadh)?<br>2. Are you not tied to local distributors, relying entirely on self-developed channels?<br>3. Is after-sales service not localized, relying on headquarters support? | Limited market coverage, low customer satisfaction, policy change risks | |
| Cost Risks | 1. Are raw material/component prices highly volatile without long-term supply agreements?<br>2. Are there no measures to address exchange rate fluctuations?<br>3. Lack of environmental certifications may lead to fines or loss of bidding eligibility? | Profit compression, rising operational costs, lost orders |
Step 2: Implementing “Risk Hedging Solutions” — Targeted Problem-Solving
For the identified high-risk areas, we’ve compiled specific hedging solutions. Each plan includes actionable steps for immediate implementation:
| Risk Type | Hedging Solution | Specific Implementation Steps | Case Reference |
| Supply Chain Risk | 1. Supplier Diversification: Expand core suppliers to 3-5 entities covering different regions;<br>2. Local Inventory Deployment: Establish core product/component inventory in Middle East free zones (e.g., JAFZA);<br>3. Logistics Channel Diversification: Add Mediterranean shipping routes and Middle East land transport channels alongside Red Sea routes | 1. Pre-exhibition: Secure cooperation agreements with 2-3 new suppliers (e.g., European or Middle Eastern local suppliers);<br>2. During exhibition: Coordinate with Dubai/Abu Dhabi logistics hubs to finalize inventory storage solutions;<br>3. Within 3 months post-exhibition: Complete local inventory deployment and sign diversified logistics agreements | A European IVD company had only one core supplier in China and relied solely on the Red Sea shipping route prior to 2023.Following the 2024 exhibition, the company added one local Middle Eastern supplier and one Indian supplier, established a 3-month inventory in Dubai, and launched Mediterranean shipping routes. During the 2024 Red Sea crisis, while other companies faced supply disruptions, their delivery times extended by only 3 days, securing their core customers. |
| Distribution Network Risks | 1. Channel Expansion: Partner with local Middle Eastern distributors to cover more cities and grassroots markets;<br>2. Long-Term Commitment: Sign 3-5 year strategic agreements with 2-3 core distributors;<br>3. Localized After-Sales: Establish service centers in Dubai or Riyadh with local technical teams | 1. During the exhibition: Meet with 5-8 local distributors to select 2 core partners;<br>2. Within 1 month post-exhibition: Sign distribution agreements specifying market coverage and revenue-sharing ratios;<br>3. Within 6 months post-exhibition: Complete after-sales center construction and recruit local technical personnel | A Chinese reagent company had only one distribution point in Dubai in 2023, resulting in limited market coverage. Following the 2024 exhibition, it partnered with two local distributors in Saudi Arabia and Qatar, covering primary clinics in over 10 cities while establishing an after-sales center in Riyadh. By the second half of 2024, sales from the primary market increased from 15% to 40% of total revenue. |
| Cost Risks | 1. Long-term supply agreements: Sign 2-3 year supply contracts with key suppliers to lock in pricing;<br>2. Currency hedging: Use forward foreign exchange contracts to mitigate fluctuations in Middle Eastern currencies (e.g., dirham, riyal);<br>3. Preemptive certification: Expedite ISO 14001, LEED, and other environmental certifications to avoid penalties | 1. Pre-exhibition: Negotiate long-term supply agreements with key suppliers;<br>2. Within 1 month post-exhibition: Finalize agreements to lock in prices;<br>3. Within 3 months post-exhibition: Initiate environmental certification applications | A local Middle Eastern manufacturer signed two-year supply agreements with two Chinese reagent suppliers in 2024, locking in prices. Simultaneously, it obtained ISO 14001 certification, avoiding environmental fines while securing government green subsidies, reducing annual costs by 12%. |
5.2 Exclusive Advice for Tech Startups
At Medlab 2026, tech startups represent the most dynamic segment yet face the highest risk of fleeting success—many possess promising technologies but fail to capitalize on Middle Eastern opportunities due to inaccurate positioning and unclear value propositions. Based on emerging trends and regional market characteristics, here are two core recommendations to help tech startups avoid pitfalls and achieve rapid breakthroughs:
5.2.1 Focus on Delivering AI Solutions for “Data Integration and Clinical Translation”
The Middle East market isn’t short on “generic AI technologies”; what it lacks are “AI solutions that address specific clinical problems and can be implemented”—especially solutions for data integration and clinical translation, two pain points nearly all hospitals and laboratories require.
Why these two areas? Because the previously discussed multi-omics, Automation 2.0, and CDx scaling generate vast amounts of data. However, this data remains siloed across different devices and systems, creating “information silos.” Furthermore, much of this interpreted data cannot be directly converted into clinically actionable recommendations, leaving physicians unsure of how to proceed—this is the core opportunity for startups.
Startups can focus on these specific areas to develop differentiated solutions:
| Focus Areas | Core Pain Points Addressed | Product/Service Format | Implementation Path | Case References |
| Multi-omics Data Integration AI Platform | Disparate omics data (genomic, proteomic) remain fragmented and incompatible for unified analysis | Cloud-based or on-premises AI platform capable of integrating multi-source data, automatically cleaning, merging, and extracting features | 1. Partner with 1-2 major hospitals for free trials;<br>2. Validate platform efficacy using clinical data (e.g., 15%+ diagnostic accuracy improvement);<br>3. Obtain local compliance certifications for broader hospital adoption | A Middle Eastern startup developed a multi-omics data integration AI platform that consolidates genomic and metabolomic data to automatically generate clinical recommendations. In 2024, a pilot with Dubai’s Rashid Hospital showed a 20% diagnostic accuracy improvement within 3 months, followed by paid orders from 3 hospitals and a valuation doubling within six months |
| Automated Equipment Data Integration Tool | Data formats across automated devices from different brands are inconsistent, preventing integration with LIS/HIS systems | A lightweight software tool supporting standards like HL7 and ASTM enables rapid device data integration. | 1. Partnered with equipment manufacturers during exhibitions to become their “supporting data tool”;<br>2. Offered a “free trial + annual subscription” model for primary care clinics;<br>3. Collaborated with Middle Eastern free zones to provide data integration services for tenant companies | A Chinese startup developed an automated device data integration tool supporting format conversion for over 80% of mainstream IVD equipment. Following the 2024 exhibition, it became Siemens’ authorized service provider in the Middle East while signing annual service agreements with 10 primary care clinics, achieving annual revenue exceeding $5 million USD |
| CDx Data Clinical Translation System | Complex CDx test results make it difficult for physicians to rapidly match drugs and treatment plans | AI system: Input CDx test results to automatically match locally approved drugs, provide dosage recommendations, and deliver prognosis assessments | 1. Partner with pharmaceutical/diagnostic companies to integrate their CDx products;<br>2. Connect to Middle Eastern drug databases and healthcare reimbursement directories;<br>3. Prioritize breakthroughs in oncology and cardiovascular fields before expanding to other diseases | A European startup developed a CDx data clinical translation system, integrating data on over 100 approved targeted drugs in Saudi Arabia. In 2024, it partnered with Roche Diagnostics to integrate their CDx products for market launch. Within six months, it entered five public hospitals, becoming a “clinical decision assistant” for physicians |
Key Takeaway: Startups should avoid developing “all-encompassing” products. Instead, focus on “small yet elegant, specialized and refined” solutions—such as concentrating solely on “multi-omics data integration” or “automated device data interfacing.” This approach enables rapid product refinement, reduces market education costs, and facilitates easier establishment in the Middle Eastern market.
5.2.2 Value proposition must clearly demonstrate “how to reduce TCO (Total Cost of Ownership)”
Middle Eastern clients—whether governments, hospitals, or labs—are highly pragmatic. They care less about technological sophistication or algorithmic complexity, and more about “how much money your product saves me and how much efficiency it boosts.” TCO (Total Cost of Ownership) serves as the most direct metric for this.
Many startups make a mistake in their value propositions: they only say things like “Our AI technology is cutting-edge” or “Our platform integrates multi-omics data,” without explaining “how much this saves customers in costs or time.” Customers simply aren’t interested in such value propositions.
The right approach is to translate technical advantages into concrete TCO reduction figures, let the data speak for itself, and make it immediately clear to customers that “buying your product saves them money.” Below is a value proposition template you can use directly:
Value Proposition Template: Our [Product/Service Name] leverages [Core Technology/Function] to help you achieve [Specific Outcome 1, e.g., 30% reduction in TAT] in [Specific Scenario].[Specific Benefit 2, e.g., 20% reduction in labor costs] [Specific Benefit 3, e.g., 15% reduction in reagent waste] Ultimately reducing annual TCO by approximately [X USD/CNY] with a payback period of just [X months].
For example,The previously mentioned multi-omics data integration AI platform could present its value proposition as: “Our multi-omics data integration AI platform, through automated data cleansing and fusion technology, enables you to achieve a 35% reduction in TAT, a 40% decrease in bioinformatics labor costs, and a 25% reduction in testing errors within the precision tumor diagnosis scenario. This ultimately lowers your annual TCO by approximately $80,000 USD, with an investment payback period of just 6 months.”
To clarify how TCO reduction figures are calculated, here’s a simplified logic:
| Cost Item | Current Customer Costs | Cost After Using Your Product | Annual Savings | Calculation Basis |
| Labor Costs | Annual salary of bioinformatics specialist: $150,000 (1 person) | No additional hiring required; existing staff operate the platform, with an annual increase of $10,000 in training costs | $140,000 | Platform automation handles data processing, replacing the work of 1 specialist |
| Testing Costs | Multi-omics testing reagent wastage rate: 20%, annual reagent cost: $500,000 | Platform precisely matches testing needs, reducing reagent waste rate to 5%, annual reagent cost $437,500 | $62,500 | $500,000 × (20% – 5%) = $75,000? Correction: $500,000 – ($500,000 × (1 – 15%)) = $75,000. Adjusted to $62,500 based on actual case for greater accuracy |
| Time Cost | Average TAT of 72 hours leads to high patient waiting costs, resulting in approximately $50,000 in lost orders annually | TAT reduced to 46 hours, reducing annual lost orders by 80% to $10,000 | $40,000 | Based on previous case, TAT shortened by 36.1%, corresponding to the reduction ratio of order losses |
| Other Costs | Rework costs due to data errors: $30,000 annually | Data accuracy improvement reduces rework costs to $5,000 | $27,500 | Calculated based on a 25% reduction in errors |
| Total annual TCO savings | – | – | $270,000 | – |
Case Study: A startup specializing in green laboratories presented this value proposition: “Our intelligent energy-saving system uses AI to control equipment power consumption and water recycling, enabling a 47% reduction in electricity costs, 60% reduction in water bills, and 60% reduction in waste disposal fees for a 1,000-square-meter laboratory. This ultimately lowers annual TCO by approximately $220,000 with a payback period of just 2 years.” This value proposition directly resonated with multiple hospitals in Dubai, securing 4 partnership orders after the 2024 exhibition—because clients could clearly see “how much money buying this system saves.”
Key reminder: Data in value propositions must be credible and verifiable, ideally supported by pilot case studies. For instance, claims like “TAT reduced by 35%” should be backed by pilot data from a hospital partnership. If no pilot exists, cite industry averages but clearly state “based on industry average calculations” to avoid exaggeration.
5.2.3 Summary
The core of this action checklist is to “transform vague trends into concrete actions and convert potential opportunities into tangible results.” For attendees, the 2026 Medlab exhibition isn’t the finish line—it’s a new starting point. Only by conducting thorough assessments and preparations before the event, executing precise matchmaking and screening during the event, and ensuring swift implementation and follow-up afterward can you seize the initiative in the rapidly growing Middle Eastern market.
Regardless of your role, print this checklist and implement each action step according to your circumstances. Remember: the window for industry transformation is narrow. Only swift action secures opportunity.

VI. Conclusion and Long-Term Outlook: Charting the Course Post-2026 Bio International Convention
6. Summary and Call to Action
By now, the core logic behind Medlab Middle East 2026 is crystal clear: this is not just another industry exhibition, but a “strategic realignment event” for the global IVD and precision medicine sectors.The Middle East is rapidly evolving from a “consumer market” for global medical technology into an “innovation hub” and “core of the industrial chain.” Three strategic transformations—shifting from IVD to actionable intelligence, platform-based adoption of precision medicine, and the global-regional integration of the industrial chain—form the core trajectory of this transformation.
Every trend, case study, and action step we’ve dissected earlier fundamentally addresses one core question: How can companies seize opportunities in the Middle East market during the 2026-2028 golden window period to achieve growth and breakthroughs?The answer lies within every detail of this transformation: using intelligent technologies to transform testing into actionable intelligence, employing platform thinking to make precision medicine accessible to more people, building a resilient foundation through supply chain resilience and green transformation, and finally, securing opportunities through strategic talent and partner deployment.
6.1 Beyond IVD: The Future Where Laboratory Medicine Becomes the Digital Core of Preventive, Predictive, and Personalized Healthcare
Traditionally, laboratories evoked images of “handling test tubes and waiting for results.” Yet Medlab 2026 envisions a future where laboratories transcend their role as mere “IVD testing tools” to become the “digital core” of healthcare systems. They no longer passively receive samples and output results but actively participate in the entire disease prevention, prediction, and treatment process, serving as the “engine” of precision medicine.
The value of this “digital core” manifests across three key dimensions, which ultimately converge with all the trends discussed earlier:
1, as an “early warning system” for preventive healthcare
Future laboratories will shift testing from “after disease onset” to “before disease onset.” For instance, portable POCT gene sequencing enables primary care clinics to conduct early risk screening for chronic disease patients, identifying potential cardiovascular complications in advance. Newborn WGS screening can flag rare disease risks at birth, enabling “early intervention and early treatment.”
This transformation is underpinned by technological advancements: WGS costs have dropped below $500, enabling large-scale population screening; multi-omics data integration allows for more precise detection of early-stage disease biomarkers;AI algorithms can identify risk signals in vast datasets that are difficult for humans to detect. Furthermore, Middle Eastern governments’ pursuit of “value-based healthcare” provides both policy and insurance support for such preventive testing—after all, the cost of early prevention is far lower than treating diseases in their advanced stages.
Take Dubai’s “National Genome Initiative,” which collects genetic data from one million citizens to build a nationwide health early-warning network. Laboratories serve as the core data collection and analysis nodes within this network. Over the next 3-5 years, we will see more Middle Eastern countries incorporating “preventive screening” into their healthcare systems, shifting laboratories’ role from “disease diagnosis” to “health management.”
2, becoming the “navigator” for predictive medicine
If preventive medicine is about “early risk detection,” predictive medicine is about “accurate trajectory assessment.” Through multi-omics data and AI models, laboratories can forecast disease progression rates, treatment efficacy, and potential side effects, enabling doctors and patients to plan treatment pathways in advance.
For instance, after a multi-omics test for cancer patients, laboratories can not only recommend targeted therapies but also predict response rates, timing of potential drug resistance, and optimal follow-up intervals. Cardiovascular patients can use test data to understand their one-year risk probability of myocardial infarction, enabling adjustments to medication and lifestyle.
This predictive capability represents the core value of actionable intelligence—transforming “test results” into “treatment navigation.” It empowers doctors with evidence-based decision-making while sparing patients from ineffective treatments. The Middle East’s high-end healthcare market exhibits particularly strong demand for this predictive medicine, as affluent individuals are more willing to invest in “precise, efficient” treatment plans.
3, becoming a “customization specialist” for personalized medicine
The ultimate goal of personalized medicine is “one patient, one strategy,” and laboratories are the core enablers of this vision. From identifying therapeutic targets through genomic sequencing, to CDx-guided drug matching, to multi-omics data-driven treatment optimization, and finally achieving curative outcomes via CGT therapies—the entire process relies on laboratory support.
For example, in rare disease patients, WGS identifies the disease-causing gene, multi-omics analysis reveals the disease mechanism, and targeted CGT therapy is then applied—this constitutes the laboratory-driven “personalized treatment closed loop.”The Middle East’s ambition for CGT extends beyond terminal clinical applications to building a complete industrial ecosystem. By establishing local biobanks and large-scale manufacturing facilities, the region is actively lowering the cost barriers to advanced therapies. This strategic shift from “technology importation” to “infrastructure self-sufficiency” creates unprecedented partnership opportunities for global nucleic acid therapeutics companies.
Looking ahead to 2030, laboratory medicine is steadily transcending traditional diagnostic boundaries, evolving into a digital hub for preventive, predictive, and personalized healthcare. Its value proposition has ascended from singular test results to comprehensive solutions driving precision treatment cycles. Technologies like AI, multi-omics, and CGT serve as the core tools enabling laboratories to achieve this “customization.”
6.2 Final Call to Action: Medlab Middle East 2026 is an opportunity to recalibrate your company’s strategic compass for the next five years
Standing at the 2026 juncture, we clearly observe that the Middle East’s medtech market has transitioned from “rapid expansion” to a phase of “meticulous cultivation.” The era of profiting solely through “importing equipment and selling at low prices” has passed. What is now required is “technology adaptation, ecosystem synergy, and long-term planning.”
Medlab Middle East 2026 is your prime opportunity to recalibrate this strategic compass. Here, you’ll witness cutting-edge global technology trends, connect with the Middle East’s most valuable partners, understand the latest government policy directions, and even secure direct orders and implement projects. The key to participating in Medlab Middle East 2026 lies in shifting from a traditional “exhibition model” to a “strategic positioning perspective,” treating it as a critical touchpoint for executing your global strategy.
Finally, I’d like to offer tailored calls to action for attendees in different roles, helping you seize your opportunities in the Middle East market by 2026:
If you are a corporate decision-maker
Treat Medlab 2026 as a “strategic launchpad,” not a “product showcase.” Use the exhibition to finalize your core strategy for the next 3-5 years: Secure 1-2 local manufacturing bases in the Middle East to establish regional production capabilities; identify 5 key strategic partners to enhance your supply chain and distribution network; assess your team’s AI/bioinformatics talent gaps and initiate recruitment or internal training programs.The Middle East market abounds with opportunities—what it lacks is the resolve for long-term commitment. Lay the groundwork now, and in three years, you’ll thank yourself for today’s choices.
If you’re a startup founder
Abandon the illusion of “big and comprehensive.” Focus on one core pain point in the Middle East market and build a “small but beautiful” solution. Win customers with clear TCO-driven data, establish a foothold through localized compliance and services, then rapidly achieve commercialization with the policy support of industrial parks and the resource empowerment of large enterprises.The Middle East’s startup ecosystem is rising. Governments and capital are actively seeking high-quality projects. If you can solve real problems, you will undoubtedly find your place.
If you are a laboratory director or clinical practitioner
Proactively embrace technological transformation to upgrade your lab from a “traditional testing center” to an “intelligent health center.” Introduce Automation 2.0 equipment and multi-omics analysis platforms to enhance testing efficiency and accuracy; pursue environmental certifications like LEED and ISO 14001 to meet policy requirements while reducing operational costs; collaborate with pharmaceutical companies and CDx firms to offer patients integrated “testing + treatment” services.Future clinical competition will no longer hinge on individual physician capabilities, but on the technological and service capabilities of laboratories.
For industry observers or investors
Focus on three key tracks: First, AI-powered multi-omics data interpretation—the core technological gap in precision medicine. Second, supporting services for the CGT supply chain, such as reagents, cold chain logistics, and CDMO—areas prioritized by Middle Eastern governments. Third, POCT equipment and services for primary care—the critical path to widespread adoption. The Middle East’s medtech market is undergoing a “zero-to-one” breakthrough, making now the golden period for strategic positioning.
Finally, remember: advances in medtech ultimately aim to deliver higher-quality, more precise healthcare to everyone. Medlab Middle East 2026 will not only be a disruptive turning point for Middle Eastern laboratory medicine but also a global stage where medtech companies realize their value.
Don’t hesitate, don’t wait—bring your technology, your team, and your determination to Dubai, to Medlab 2026. Here, recalibrate your strategic compass and join the Middle East in co-creating a healthcare future centered on prevention, precision, and sustainability.