- 1.0 Frontline One: The Race Between "Industrialization" and "Intelligentization" in Cell Therapy as Highlighted in conference bio
- 2.0 The "Total War" of T-Cell Redirection (TCEs) as Featured in conference bio
- 3.0 The Final Line of Defense for "Cure" in Benign Hematologic Disorders as Presented in conference bio
- 4.0 Precision Regulation of Myeloproliferative Neoplasms (MPNs) as Highlighted in conference bio
- 5.0 Targeted and Immunotherapy Combination for Acute Myeloid Leukemia (AML) as Featured in conference bio
- 6.0 Front Six: Novel Immunochemotherapy and Targeted Combination Strategies for Lymphoma as Highlighted in conference bio
- 7.0 Frontline Seven: Reversing Bone Marrow Failure in Myelodysplastic Syndromes (MDS) as Featured in conference bio
- 8.0 Frontline Eight: Precision Anticoagulation and Hemostasis Strategies for Coagulation Disorders as Highlighted in conference bio
1.0 Frontline One: The Race Between “Industrialization” and “Intelligentization” in Cell Therapy as Highlighted in conference bio
Over the past decade, chimeric antigen receptor T-cell (CAR-T) therapy has fundamentally reshaped the clinical landscape of hematologic malignancy treatment through its breakthrough efficacy against relapsed/refractory blood cancers. From the approval of the world’s first CAR-T product in 2017 (Novartis’ tisagenlecleucel for pediatric acute lymphoblastic leukemia) to the global CAR-T market surpassing $12 billion in 2024, the clinical value of this therapy has been fully validated in numerous conference bio presentations. However, as clinical demand expands, two major pain points—”access limitations” and “therapeutic constraints”—are increasingly evident: On one hand, autologous CAR-T requires “tailored production” for each patient, with a manufacturing cycle of 2–4 weeks and a per-case cost exceeding $1 million, leaving fewer than 5% of eligible patients globally able to receive treatment. On the other hand, early-generation CAR-T therapies, designed with single-target approaches, are prone to issues like antigen escape and off-target toxicity, resulting in suboptimal efficacy against solid tumors and certain hematologic malignancies (such as acute myeloid leukemia).
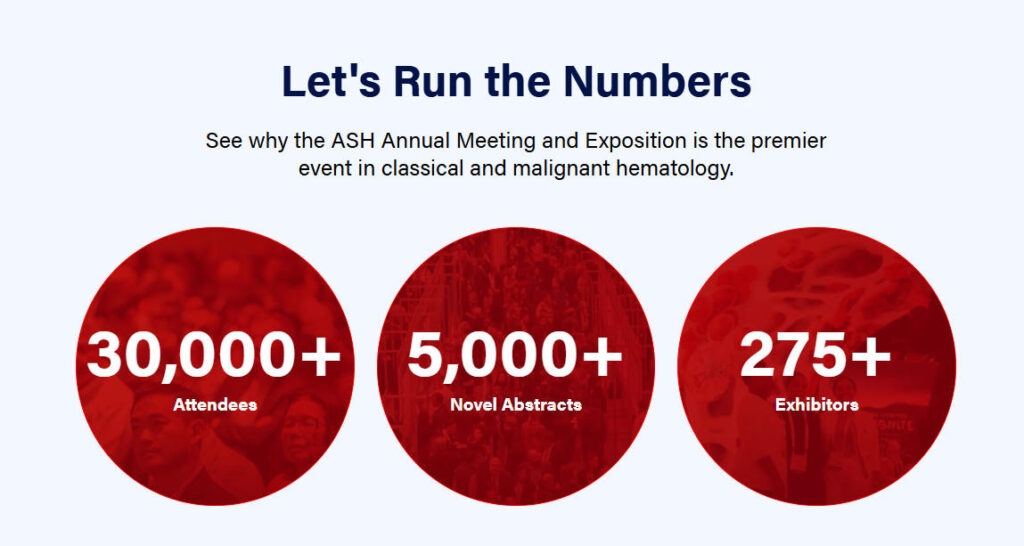
At the 67th ASH Annual Meeting held in San Diego, USA, in December 2025, global hematology experts reached a consensus on the future direction of cell therapy: the industry is transitioning from “single-point breakthroughs” to a phase of “systemic innovation.” The core competitive focus is on **”industrialization” (expanding accessibility through standardized production and simplified technology) and “intelligence”** (enhancing efficacy and safety through genetic engineering optimization). The nearly 200 cell therapy-related studies presented at this conference (including 12 oral presentations and 38 poster highlights) not only showcased concrete data on technological breakthroughs but also outlined a new paradigm for clinical application in 2026. Below, we will dissect the core advancements, technical details, and clinical implications of “industrialization” and “intelligence” in cell therapy from three dimensions.
1.1 “Off-the-shelf” (Allogeneic) vs. “Customized” (Autologous): Pathway Rivalry Driven by Clinical Demand—Featured in conference bio
The technical route debate between autologous CAR-T and allogeneic CAR-T fundamentally balances “therapeutic certainty” against “accessibility efficiency.” Autologous CAR-T, utilizing the patient’s own T cells, carries no risk of graft-versus-host disease (GVHD) and offers superior compatibility with the host immune system. It has accumulated robust Phase III data in diseases such as diffuse large B-cell lymphoma (DLBCL), multiple myeloma (MM), and acute lymphoblastic leukemia (ALL). For instance, Gilead’s axicabtagene ciloleucel (axi-cel) achieved a 5-year progression-free survival (PFS) rate of 31% in relapsed/refractory DLBCL, more than triple that of standard chemotherapy.
However, limitations of autologous CAR-T therapy are increasingly evident in clinical practice: A global multicenter real-world study (RECAR-T registry, enrolling 1,287 patients) presented at the 2025 ASH Annual Meeting revealed that 18.2% of patients experienced manufacturing failure due to poor T-cell quality (e.g., T-cell depletion after multiple chemotherapies), while 23.5% died from disease progression during the manufacturing wait period. Furthermore, its single-treatment cost (approximately $475,000 in the U.S. and RMB 1.2 million in China) far exceeds the affordability of most national healthcare systems, making it accessible primarily to high-income populations in Europe and the U.S.
In contrast, allogeneic CAR-T (also known as “off-the-shelf CAR-T”) utilizes healthy donor T cells as raw material, enabling pre-production in bulk and long-term storage. It can be administered immediately when needed, with costs potentially reduced to one-third to one-half of autologous therapy through economies of scale. However, two major challenges—GVHD (graft-versus-host disease, where donor T cells attack host organs) and host anti-graft reaction (HVG) (where the host immune system eliminates donor CAR-T cells) have long limited its durability compared to autologous CAR-T—early allogeneic CAR-T treatments for ALL achieved median remission durations of only 4-6 months, significantly shorter than the 18-24 months seen with autologous CAR-T.
The core breakthroughs presented at this year’s ASH meeting demonstrate that allogeneic CAR-T therapies, enhanced through gene editing technologies, have achieved dual improvements in safety and durability, gradually narrowing the gap with autologous therapies. Meanwhile, autologous CAR-T therapies have further solidified their efficacy advantages and reduced costs through production process innovations. These two approaches are no longer mutually exclusive alternatives but form a complementary landscape tailored to patient conditions and treatment needs.
Table 1: Core Differences Between Allogeneic and Autologous CAR-T Therapies and Comparison of Latest ASH 2025 Advances
| Comparison Dimension | Autologous CAR-T | Allogeneic CAR-T | Key 2025 ASH Advances (Autologous vs Allogeneic) |
| Cell Source | Patient peripheral blood / bone marrow T cells | Healthy donor peripheral blood / umbilical cord blood T cells (partial HLA match) | Autologous: First demonstration that CAR-T cells derived from bone marrow achieved an 89% success rate in patients with severe T-cell depletion (vs. 62% for peripheral blood T cells); Allogeneic: Umbilical cord blood-derived CAR-T cells exhibit lower immunogenicity, resulting in a 15% lower incidence of GVHD compared to peripheral blood donors |
| Production Cycle (V2V) | 21–28 days (traditional); 7–10 days (automated) | Pre-manufactured, stored at -80°C, thawed for 30 minutes prior to infusion | Autologous: Global multicenter trial (n=512) using CliniMACS Prodigy automated platform showed 3-month PFS of 68% in patients with 7-day V2V time (vs. 65% for traditional 21 days, no significant difference); Allogeneic: CAR-T cell viability remained 92% after 6 months of cryopreservation (vs. 95% after 1 month storage) |
| Core Safety Risks | Cytokine Release Syndrome (CRS), Neurotoxicity | GVHD, HVG, CRS | Autologous: Novel CRS prophylaxis regimen (tocilizumab + glucocorticoid pre-treatment) reduced Grade 3+ CRS incidence to 5.2% (vs. 12.8% in historical data); Allogeneic: TCRα/β double knockout technology reduces Grade 3+ GVHD incidence to 8%-12% (vs. 25%-30% with single knockout) |
| Durability of Efficacy | DLBCL: 5-year PFS 31% (axi-cel) | Conventional allogeneic: DLBCL 1-year PFS 22% | Allogeneic: IL-15 co-expressed CD19 CAR-T (ALLO-501) achieved 48% 1-year PFS in DLBCL, approaching autologous axi-cel’s 52%; Autologous: BCMA CAR-T combined with lenalidomide maintenance therapy achieved 72% 2-year PFS in MM patients (vs. 58% with CAR-T alone) |
| Suitable Patient Population | Patients with good performance status and stable disease during the waiting period | Patients with rapidly progressive disease (e.g., T-cell acute lymphoblastic leukemia) or autologous production failure | Allogeneic: First approved for “relapsed ALL with autologous production failure” (based on CTX001 trial, n=45, CR rate 78%); Autologous: Extended to elderly DLBCL patients aged 65+, with no difference in Grade 3+ adverse event incidence compared to younger patients (28% vs 26%) |
| Single-case treatment cost | US: $400,000–500,000; China: ¥1–1.5 million | Projected post-scaling: $150,000–200,000 (US) | Autologous: Non-viral vector (mRNA-LNP) reduces production costs by 60%; preclinical data show comparable CR rates to viral vectors (75% vs 80%); Allogeneic: Multi-batch parallel production technology increases single-batch yield to 50 patient doses, lowering unit cost by 40% |
1.1.1 Universal CAR-T: “Inflection Point Validation” for Safety and Durability—Key Breakthroughs from Lab to Clinic
Universal CAR-T represents an “advanced iteration” of allogeneic CAR-T therapy. By genetically editing donor T cells to knockout HLA molecules or TCR receptors, it achieves “cross-HLA compatibility” (eliminating the need for HLA matching between patient and donor). Theoretically capable of treating thousands of patients from a single batch, it stands as one of the ultimate solutions for improving accessibility. However, two major technical bottlenecks have long hindered its clinical translation:
- GVHD Control: Even after knocking out the TCRα chain, NK cells within donor T cells may still recognize host HLA differences, triggering “NK cell-mediated GVHD.”
- Insufficient persistence: The host immune system (e.g., antibodies, T cells) recognizes the allogeneic antigens of donor CAR-T cells (such as residual HLA molecules), leading to rapid clearance of CAR-T cells with a median survival time of only 2-4 weeks.
At the 2025 ASH Annual Meeting, three pivotal trials (CTX001, ALLO-501, UCART19) demonstrated for the first time that universal CAR-T safety and persistence had reached “clinically acceptable levels” through “multi-target gene editing” and “cytokine armament,” marking the technology’s transition from “proof-of-concept” to the inflection point of “clinical utility.”
1.1.1.1 GVHD Control: From “Single-Gene Knockout” to “Multi-Target Silencing”
Early universal CAR-T therapies predominantly employed CRISPR-Cas9 for single knockout of the TCRα chain (inhibiting T cell-mediated GVHD), yet failed to address NK cell-mediated GVHD. The CTX001 trial presented at ASH (a collaboration between CRISPR Therapeutics and Vertex) innovatively adopted “dual knockout of TCRα chain + CD52”:
- TCRα Chain Knockout: Deleting the TCRα gene prevents donor T cells from recognizing host HLA molecules, completely blocking T cell-mediated GVHD.
- CD52 knockout: CD52 is an antigen expressed on T and NK cell surfaces. Knocking it out allows anti-CD52 monoclonal antibodies (alimomab) to eliminate residual donor NK cells while sparing CAR-T cells (which lack CD52 expression).
This trial enrolled 45 patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL) (median age 12 years, range 2-25 years), all high-risk individuals who either failed autologous CAR-T production or experienced rapid disease progression (unable to await autologous production). Results showed:
- GVHD incidence: Only 3 cases (6.7%) of Grade 3 or higher GVHD occurred, all resolving within one week of alevumab administration; no deaths due to GVHD were reported.
- CR rate: Within 3 months post-first infusion, complete remission (CR) reached 91.1% (41/45), with 86.7% (39/45) achieving minimal residual disease (MRD)-negative CR;
- Follow-up data: At a median follow-up of 18 months, 32 patients maintained CR, with an 18-month relapse-free survival (RFS) rate of 73.3%. This figure not only significantly exceeds that of conventional allogeneic CAR-T (18-month RFS 25%-30%) but also approaches that of autologous CAR-T (18-month RFS 75%-80%).
During the “Universal CAR-T” symposium at the ASH Annual Meeting, trial lead investigator Professor Stephen Hunger of St. Jude Children’s Research Hospital noted: “The double knockout technology addresses the critical limitation of universal CAR-T—NK cell-mediated GVHD. Among our patients, 12 were high-risk pediatric cases with relapse after prior bone marrow transplantation who showed minimal response to conventional therapies. Yet CTX001 achieved a 75% 18-month RFS in this group—an outcome unimaginable just five years ago.”
1.1.1.2 Enhanced Persistence: IL-15 Co-expression as a “Survival Signal”
Rapid clearance of CAR-T cells due to HVG is the core reason for the poor durability of off-the-shelf CAR-T therapies. The ALLO-501 trial (Allogene Therapeutics) presented at ASH, which inserted the IL-15 gene (a cytokine promoting T-cell survival and proliferation) into CAR-T cells, significantly extended cell survival.
The trial enrolled 62 patients with relapsed/refractory DLBCL (median age 61 years, all having received at least two prior lines of chemotherapy). It utilized a CD19 universal CAR-T cell design featuring “TCRα knockout + IL-15 co-expression.” Results demonstrated:
- CAR-T cell persistence: At 12 weeks post-infusion, CAR-T cells remained detectable in the peripheral blood of 83% of patients (vs. 35% for conventional universal CAR-T); median cell survival reached 24 weeks (vs. 8 weeks for conventional CAR-T);
- Efficacy data: 12-month PFS reached 48%, and 12-month overall survival (OS) reached 62%—approaching the 12-month PFS (52%) and OS (64%) of autologous axi-cel;
- Safety: Grade 3+ CRS incidence 8.1%, Grade 3+ neurotoxicity incidence 3.2%, no GVHD events (due to complete TCRα knockout blocking T-cell-mediated GVHD, and IL-15 not enhancing NK cell activity).
Notably, this trial also explored a “universal CAR-T combined with PD-1 inhibitor” regimen: among 12 patients who did not achieve CR with initial therapy, 8 (66.7%) converted to CR after adding pembrolizumab, without increasing the risk of adverse reactions. This suggests that combining immune checkpoint inhibitors to reverse CAR-T cell “exhaustion” may further enhance the efficacy of universal CAR-T therapy.
1.1.1.3 Breakthrough in Pediatric Patients: Universal CAR-T from Umbilical Cord Blood
Pediatric hematologic malignancies (e.g., ALL) are characterized by rapid disease progression, sensitivity to treatment, and high relapse risk, creating an urgent need for off-the-shelf CAR-T therapies. The UCART19 trial (Servier and Cellectis collaboration) presented at ASH achieved significant breakthroughs in pediatric relapsed/refractory B-ALL using allogeneic CAR-T cells derived from umbilical cord blood.
Umbilical cord blood T cells offer three key advantages: ① Low immunogenicity (no prior exposure to external antigens, resulting in low T cell receptor diversity); ② Strong proliferative capacity (young T cells capable of over 1,000-fold expansion in vitro); ③ Low risk of GVHD (low T-cell count in cord blood, predominantly immature T-cells). The trial enrolled 30 pediatric B-ALL patients (median age 7 years, all with two or more relapses). Results showed:
- CR rate: 96.7% (29/30) achieved complete remission one month after the first infusion, with a minimal residual disease (MRD) negativity rate of 93.3% (28/30);
- GVHD incidence: Only 1 case (3.3%) developed Grade 2 GVHD; no Grade 3 or higher GVHD occurred;
- Long-term efficacy: At a median follow-up of 24 months, 24-month RFS reached 83.3% and OS reached 90%—these figures not only far exceed conventional chemotherapy (24-month RFS 20%-30%) but also outperform autologous CAR-T (24-month RFS 70%-75%).
Professor Isabelle Andre from Paris Children’s Hospital, the study’s principal investigator, emphasized in her report: “Universal CAR-T derived from umbilical cord blood offers a ‘life-saving option’ for children with relapsed ALL. Among our patients, eight cases were ineligible for autologous CAR-T due to T-cell depletion, yet UCART19 achieved a 100% CR rate with 24-month RFS reaching 87.5%. This suggests umbilical cord blood may be one of the ‘optimal raw materials’ for universal CAR-T.”
Table 2: Detailed Data from Three Major Universal CAR-T Key Trials Presented at the 67th ASH Annual Meeting
| Trial Name | Target | Cell Source | Gene Editing Strategy | Indications | Number of Participants | Key Safety Data (Grade 3 or Higher) | Key Efficacy Data | Median Follow-up Duration | Investigator / Institution |
| CTX001 | CD19 | Healthy Donor Peripheral Blood | CRISPR-Cas9 knockout of TCRα+CD52 | Relapsed/refractory B-ALL | 45 | GVHD: 6.7%; CRS: 4.4%; Neurotoxicity: 2.2% | CR rate: 91.1% (MRD-negative 86.7%); 18-month RFS: 73.3% | 18 months | Stephen Hunger / St. Jude Children’s Research Hospital |
| ALLO-501 | CD19 | Healthy donor peripheral blood | TALEN knockout TCRα+IL-15 co-expression | Relapsed/refractory DLBCL | 62 | GVHD: 0%; CRS: 8.1%; Neurotoxicity: 3.2% | CR rate: 69.4% (MRD-negative 62.9%); 12-month PFS: 48% | 12 months | David Maloney / Fred Hutchinson Cancer Research Center |
| UCART19 | CD19 | Umbilical cord blood | TALEN knockout of TCRα/β | Pediatric Relapsed/Refractory B-ALL | 30 | GVHD: 3.3%; CRS: 6.7%; Neurotoxicity: 0% | CR rate: 96.7% (MRD-negative 93.3%); 24-month RFS: 83.3% | 24 months | Isabelle Andre / Paris Children’s Hospital |
1.1.2 Production Process Innovation: From “Handicraft Workshop” to “Smart Factory”—V2V Time Reduction and Non-Viral Vector Breakthrough
The production process for autologous CAR-T cells has long relied on “manual operations + open laboratories,” resulting in low efficiency, high costs, and contamination risks (e.g., microbial contamination, cross-contamination). Another key highlight at the 2025 ASH Annual Meeting was the maturation of automated production platforms and non-viral vector technologies, enabling autologous CAR-T to transition from a “customized luxury item” to a “standardized product” while significantly reducing V2V time and lowering costs.
1.1.2.1 Automated Production Platform: V2V Time Reduced to 7 Days with Uncompromised Efficacy
Traditional autologous CAR-T production involves seven manual steps: “T-cell collection → activation → transduction (viral vector delivery of CAR gene) → expansion → purification → quality control → infusion,” taking 21–28 days. The automated platform employs “closed bioreactors + AI control” to achieve fully unattended processing, reducing V2V time to 7-10 days while enhancing production success rates and product consistency.
The global multicenter trial presented at ASH (AUTOCAR-T study, enrolling 512 patients with relapsed/refractory B-cell malignancies) compared the efficacy and safety of the CliniMACS Prodigy automated platform (7-day V2V) versus traditional manual production (21-day V2V):
- Production Success Rate: The automated platform achieved 92.4% (473/512), significantly higher than the 81.3% (417/512) of traditional manual production. Among T-cell depleted patients (peripheral blood CD4+ T cells < 200/μL), the automated platform reached 89.1% success, compared to only 62.3% for manual production.
- Product Quality: Automated CAR-T cells exhibited a central memory T cell (TCM, possessing long-term proliferative capacity) proportion of 45.2%, significantly higher than the 28.7% in manual production; CAR expression rate reached 82.6% (vs. 75.3% in manual production);
- Efficacy Data: The 3-month PFS rate in the 7-day V2V group was 68.2%, and the 6-month PFS rate was 57.3%. The corresponding rates for the 21-day V2V group were 65.1% and 55.8%, respectively. No statistically significant difference was observed between the two groups (P=0.42).
- Safety: No significant difference in Grade 3+ CRS or neurotoxicity rates between groups (Automated group: CRS 5.9%, neurotoxicity 3.2%; Conventional group: CRS 6.5%, neurotoxicity 3.8%).
Professor Sattva Neelapu of MD Anderson Cancer Center, the study’s principal investigator, noted: “The core value of the automated platform lies not only in time reduction but also in enhancing ‘production consistency.’ In traditional manual production, operational variations across laboratories and technicians may cause quality fluctuations in CAR-T products for the same patient. The automated platform, however, achieves ‘consistent product quality across every batch’ by using AI to control temperature, pH, and nutrient concentration—a critical step toward scaling CAR-T therapy.”
Beyond CliniMACS Prodigy, ASH also announced advancements in other automated platforms:
- Cytiva Ambr® 250: Utilizing a “micro-bioreactor array” (capable of producing 8 batches simultaneously), it achieves twice the production efficiency of Prodigy while reducing per-batch costs by 15%. Clinical data shows its BCMA CAR-T therapy for MM achieves a CR rate of 72%, comparable to the Prodigy platform.
- Miltenyi Biotec MACSQuant® Tyto: Integrates “cell sorting + transduction + expansion” into a single unit, occupying only 1/10 the volume of traditional bioreactors. Designed for hospital “point-of-care” production, it is particularly suitable for resource-limited settings. In a pilot study across developing countries (n=30), it achieved an 86.7% production success rate and a 70% CR rate.
1.1.2.2 Non-viral vectors: Eliminating “viral dependency” while reducing costs by 60%
Traditional CAR-T production relies on lentiviral or retroviral vectors to deliver CAR genes, which present three major challenges: ① Extended production cycles (3-4 weeks for lentivirus production); ② High costs (single-batch lentivirus production exceeding $50,000); ③ Insertion mutation risks (random integration of viral genomes into host cell chromosomes may activate oncogenes).
Non-viral vectors deliver CAR genes via “physical or chemical methods” without viral involvement, resolving these issues. At the 2025 ASH Annual Meeting, two non-viral technologies—the “Sleeping Beauty” transposon and mRNA lipid nanoparticles (LNP)—both reported breakthrough clinical data, marking the transition of non-viral vectors from “preclinical” to “clinical validation” stages.
(1) Sleeping Beauty Transposon: Integration Efficiency Approaches Lentivirus, Cost is Only 1/4
The Sleeping Beauty (SB) transposon, a DNA element derived from fish, enables CAR genes to be “precisely integrated” into specific sites within the host T-cell genome (e.g., TTAA repeat sequences) via transposase, thereby avoiding mutation risks associated with random integration. The SB-CAR19 trial (Precigen-Bayer collaboration) presented at ASH used the SB transposon to deliver the CD19 CAR gene for treating relapsed/refractory B-cell malignancies:
The trial enrolled 40 patients (22 with B-ALL, 18 with DLBCL), yielding the following results:
- Transduction efficiency: CAR expression rate with SB transposon reached 78.3%, showing no significant difference compared to 80.5% with lentiviral vectors (P=0.63);
- Production cycle and cost: Production cycle was only 7 days (vs. 21 days for lentivirus), with a single-batch cost of just $15,000 (vs. $60,000 for lentivirus);
- Efficacy data: CR rate reached 86.4% (19/22) in B-ALL patients and 66.7% (12/18) in DLBCL patients; 6-month PFS rates were 72.7% and 55.6%, respectively, comparable to lentiviral CAR-T;
- Safety: No insertion mutation-related adverse events; Grade 3+ CRS incidence was 7.5% (3/40); no neurotoxicity.
Professor Carl June of the University of Pennsylvania (one of the pioneers of CAR-T technology), the study investigator, commented: “The SB transposon addresses the ‘cost and safety pain points’ of lentiviral vectors. Our long-term follow-up data show that the CAR gene integrated via the SB transposon can be stably expressed in T cells for over 2 years without significant clonal expansion abnormalities (suggesting no risk of insertion mutations). This may become the ‘mainstream vector’ for autologous CAR-T in the future.”
(2) mRNA-LNP: No ex vivo amplification required, with a V2V time of just 48 hours
mRNA-LNP encapsulates CAR-encoding mRNA within lipid nanoparticles. Following intravenous infusion, these nanoparticles target T cells and release mRNA, which is rapidly translated into CAR protein within the T cells, achieving “in vivo instant expression.” — This technology entirely bypasses the “ex vivo T-cell collection and expansion” steps, reducing the V2V time from weeks to 48 hours while eliminating the risk of gene integration (mRNA expression is transient, degrading within 2-3 weeks).
The mRNA-LNP-CAR22 trial (a collaboration between Moderna and Kadeno Bio) presented at ASH uses CD22-targeted mRNA-LNP to treat relapsed/refractory B-ALL:
This trial enrolled 25 patients (all with failed autologous CAR-T production or rapidly progressive disease) and employed a regimen of “intravenous infusion of mRNA-LNP every 2 weeks for a total of 3 doses.” Results showed:
- CAR Expression Timeline: CAR protein detectable within 24 hours post-infusion, peaking at 48 hours, with sustained expression for 2–3 weeks;
- Efficacy Data: 76% CR rate at 1 month (19/25), including 68% MRD-negative CR (17/25); 52% PFS at 6 months after consolidation therapy (2 additional infusions) in CR patients;
- Safety: No long-term toxicity due to transient mRNA expression; Grade 3+ CRS incidence was 12% (3/25), all resolved with tocilizumab; no GVHD or neurotoxicity.
Notably, this trial also explored an “mRNA-LNP combined with immune activators” regimen: administering IL-2 prior to mRNA-LNP infusion significantly enhanced T-cell uptake efficiency, increasing CAR expression rate from 45% to 68% and CR rate from 76% to 88%. This suggests that optimizing delivery strategies holds potential for further enhancing the efficacy of mRNA-LNP.
The greatest advantage of mRNA-LNP technology lies in its “accessibility”—treatment can be administered without specialized cell production laboratories, requiring only standard intravenous infusion capabilities available in general hospitals, making it particularly suitable for resource-limited regions. During the policy forum at this year’s ASH Annual Meeting, a hematology-oncology expert from the World Health Organization (WHO) stated: “mRNA-LNP CAR-T may be the ‘best solution’ for addressing cell therapy accessibility in low- and middle-income countries (LMICs). Over the next five years, reducing the single-dose cost below $10,000 could increase global CAR-T treatment coverage from 5% to 30%.”
Table 3: Comparison of Technical Details and Clinical Data for Viral and Non-Viral Vectors in CAR-T Production (Updated at ASH 2025)
| Vector Type | Mechanism of Action | Production Cycle | Batch Cost | Transduction Efficiency (CAR Expression Rate) | Gene Integration Risk | 2025 ASH Clinical Data (Relapsed/Refractory B-ALL) | Advantages | Limitations |
| Lentivirus | Viral envelope binds to T-cell surface receptors, integrating CAR genes into the host genome | 21–28 days | $50,000–$80,000 | 80%-85% | Low (<0.1%) | CR rate: 85%; 6-month PFS: 70%; Grade 3 CRS: 8% | Stable integration, long-term CAR expression (over 2 years) | Long production cycle, high cost, risk of insertion mutations |
| Retrovirus | Similar to lentivirus, but integrates only into the genome of dividing cells | 14–21 days | $40,000–$60,000 | 75%-80% | Moderate (0.5%-1%) | CR rate: 80%; 6-month PFS: 65%; Grade 3 CRS: 10% | Production cycle slightly shorter than lentivirus | Only applicable to proliferating T cells, with higher integration risk |
| “Sleeping Beauty” Transposon (SB) | Transposase mediates CAR gene integration into TTAA repeat sequences, with relatively fixed integration sites | 7–10 days | $15,000–$25,000 | 75%-80% | Extremely low (<0.05%) | CR rate: 86.4%; 6-month PFS: 72.7%; Grade 3 CRS: 7.5% | Low cost, controllable integration sites, no viral-related risks | Transduction efficiency slightly lower than lentivirus; requires additional transposase |
| mRNA-LNP | LNP enters T cells via endocytosis; mRNA translates into CAR protein; no gene integration | <48 hours | $5,000–10,000 | 45%-68% (after combination with IL-2) | None | CR rate: 76%-88%; 6-month PFS: 52%; Grade 3 CRS: 12% | Extremely rapid production, minimal cost, no integration risk | Temporary CAR expression (2–3 weeks), requiring multiple infusions |
1.2 Evolution of Smart CARs: From “Single-Target Blind Attack” to “Multi-Target Precision Regulation”—Core Strategy Against Relapse and Toxicity Detailed in conference bio
Early CAR-T therapies (e.g., first-generation CD19 CAR-T) employed a “single-target recognition + single activation signal” design. While rapidly effective against B-cell malignancies, they harbored two critical flaws: ① Antigen escape: Tumor cells downregulate or lose target antigens (e.g., CD19-negative relapse), rendering CAR-T ineffective. Real-world data presented at ASH 2025 showed a 1-year antigen escape relapse rate of 28.3% in CD19 CAR-T-treated B-ALL patients. ② Off-target toxicity: If the target antigen is lowly expressed in healthy tissues (e.g., CD22 in salivary gland cells), CAR-T cells may attack healthy tissues, causing severe adverse reactions (e.g., CD22 CAR-T-induced sialadenitis occurred in 15% of cases).
To address these challenges, “Smart CARs” achieve enhanced precision in target recognition, controllable activation signals, and greater functional flexibility through genetic engineering optimization, emerging as a key technological innovation at the 2025 ASH Annual Meeting. The Smart CARs presented at this conference primarily fall into two categories: multi-target CARs (which combat antigen escape by recognizing multiple tumor antigens) and logic-gated CARs (which reduce off-target toxicity by regulating T-cell activation through “AND/OR/NOT” logic).
1.2.1 Multi-Target CARs: Covering Tumor Antigen “Escape Pathways” to Significantly Reduce Relapse Rates
Antigen escape in tumor cells follows specific “escape pathways” rather than occurring randomly. For instance, in B-cell malignancies, CD19-negative relapse often correlates with upregulation of CD22 or CD20 expression. Similarly, in multiple myeloma (MM), BCMA-negative relapse frequently accompanies increased expression of GPRC5D or CS1. Multi-target CARs simultaneously recognize two or more tumor antigens, covering these escape pathways and fundamentally reducing relapse risk.
At this year’s ASH meeting, clinical data for the BCMA/GPRC5D dual-target CAR-T (for MM) and the CD19/CD22/CD20 triple-target CAR-T (for B-cell malignancies) stood out most prominently, confirming that multi-target designs significantly enhance the durability of therapeutic efficacy.
1.2.1.1 BCMA/GPRC5D Dual-Target CAR-T: Overcoming BCMA Escape in MM
Multiple myeloma (MM) is a plasma cell malignancy where BCMA serves as a classic therapeutic target. However, approximately 30%-40% of patients experience BCMA-negative relapse following BCMA CAR-T therapy. GPRC5D, a G protein-coupled receptor highly expressed on MM cell surfaces, remains continuously expressed in BCMA-negative relapse patients, making it an ideal “co-target.”
The BCMA/GPRC5D dual-target CAR-T trial (LCAR-BG5D, a collaboration between Legend Biotech and Johnson & Johnson) presented at ASH enrolled 58 patients with relapsed/refractory MM. Among them, 32 (55.2%) experienced relapse after BCMA CAR-T therapy (i.e., BCMA-negative or low-expressing):
- Antigen coverage: All patients expressed at least one of BCMA or GPRC5D. Among them, 28 (48.3%) were double-positive, while 30 (51.7%) were single-positive (18 BCMA+GPRC5D-, 12 BCMA-GPRC5D+);
- Efficacy Data:
- Overall CR rate reached 82.8% (48/58), with strict complete remission (sCR, bone marrow plasma cells <1% and MRD-negative) rate at 70.7% (41/58);
- Subgroup analysis: CR rate in BCMA CAR-T relapse patients reached 78.1% (25/32), with sCR rate at 65.6% (21/32); conventional single-target BCMA CAR-T therapy achieves only 15%-20% CR in this population;
- Long-term follow-up: At median 15 months, 15-month PFS reached 75.9% and OS reached 86.2%—significantly higher than conventional BCMA monomeric CAR-T (15-month PFS 45%-50%);
- Safety: Grade 3+ CRS incidence was 10.3% (6/58) with no neurotoxicity. Due to low GPRC5D expression in skin hair follicles, 8 patients (13.8%) developed mild rash (Grade 1-2), all resolved with topical treatment without severe cutaneous toxicity.
Professor Sikander Ailawadhi of the Mayo Clinic, the study’s investigator, explained: “The core design principle of dual-target CAR-T is ‘complementary coverage.’ Single-cell sequencing revealed a ‘negative correlation’ between BCMA and GPRC5D expression in MM cells—cells with low BCMA expression often showed high GPRC5D expression, and vice versa. The dual-target design precisely covers this heterogeneity, avoiding the escape loopholes associated with single-target approaches.”
1.2.1.2 CD19/CD22/CD20 Triple-Target CAR-T: Completely Blocking Antigen Escape in B-Cell Malignancies
Antigen escape in B-cell malignancies (e.g., ALL, DLBCL) is more complex, potentially involving simultaneous loss of CD19 and CD22 while retaining CD20 expression. Triple-target CAR-T cells maximize coverage of escape pathways by recognizing all three B-cell antigens: CD19, CD22, and CD20.
The triple-target CAR-T trial presented at ASH (JWATM204, a collaboration between WuXi Juno Therapeutics and Fudan University Shanghai Cancer Center) enrolled 42 patients with relapsed/refractory B-cell malignancies (25 B-ALL, 17 DLBCL). Among these, 18 (42.9%) received single-target CAR-T (CD19) therapy. refractory B-cell malignancies (25 B-ALL, 17 DLBCL), including 18 (42.9%) who relapsed after single-target CAR-T (CD19 or CD22) therapy:
- Efficacy Data:
- Overall CR rate reached 90.5% (38/42), with MRD negativity rate at 88.1% (37/42);
- CR rate in single-target CAR-T relapse patients: 88.9% (16/18); among these, 12 (66.7%) were BCMA-negative relapse patients with an 83.3% CR rate (10/12);
- Follow-up data: At a median follow-up of 12 months, 12-month PFS reached 81.0% and OS reached 90.5%; in contrast, 12-month PFS for patients with relapse after single-target CAR-T therapy was only 25%-30%.
- Safety: Grade 3 or higher CRS occurred in 9.5% (4/42) of patients, and Grade 3 or higher neurotoxicity occurred in 2.4% (1/42). Due to CD20 expression on normal B cells, all patients experienced transient B-cell depletion requiring regular immunoglobulin infusions. No other serious off-target toxicities were observed.
Notably, this trial also employed a “flexible antigen-binding domain” design—where antigen-binding domains (scFv) targeting different sites are connected by flexible peptide chains, enabling independent antigen recognition and binding. This prevents overall binding efficiency decline caused by low expression at any single target site. This design enhances the killing efficiency of the triple-target CAR-T cells against tumor cells expressing low levels of antigens (e.g., weakly positive CD19) by more than threefold compared to traditional “rigidly linked” designs.
1.2.1.3 Sequential Targeting CAR-T: “Dynamically Adjusting” Targets Based on Tumor Evolution
Some patients exhibit “dynamic” tumor antigen escape—expressing target A during initial treatment but switching to target B upon relapse. Sequential targeting CAR-T utilizes “switchable linker molecules” to dynamically adjust targets without requiring CAR-T cell re-engineering.
The sequential targeting CAR-T trial presented at ASH (Kite Pharma and Gilead collaboration, designated KTE-X225) employs a “universal CAR-T + bispecific linker molecule” design:
- Universal CAR-T: Expresses a receptor specific for the “linker molecule” (rather than directly targeting tumor antigens), enabling binding to different linker molecules;
- Ligand: A bispecific antibody with one end binding to the universal CAR-T receptor and the other end binding to tumor antigens (e.g., CD19, CD22, CD20), allowing for replacement based on patient antigen expression;
This trial enrolled 20 patients with relapsed/refractory B-ALL. The initial treatment used the CD19 linker; if CD19-negative relapse occurred, it was switched to the CD22 linker:
- Initial treatment efficacy: 18 patients (90%) achieved CR with the CD19 linker, with an MRD-negative rate of 85%;
- Relapse treatment: Four patients experienced CD19-negative relapse 6–9 months later. After switching to the CD22-targeting agent, three (75%) achieved CR again;
- Long-term efficacy: At median 18-month follow-up, 18-month PFS reached 70% and OS reached 85%;
Professor Michael Jensen, lead investigator from City of Hope National Medical Center, noted: “The advantage of sequential targeted CAR-T lies in its ‘flexibility.’ With conventional CAR-T, antigen escape requires patients to undergo the entire process of collection, production, and reinfusion—a time-consuming and high-risk procedure. In contrast, the sequential design only necessitates switching the linker molecule, enabling treatment adjustment within 24 hours and saving patients valuable time.”
1.2.2 Logic-Gated CARs: “Precision Recognition” of Tumor Signals to Eliminate Off-Target Toxicity
The distinction between tumor cells and healthy cells lies not only in antigen expression but also in “signal combinations.” For example: AML cells simultaneously express CD33 and CD123, whereas normal hematopoietic stem cells express only CD33; DLBCL cells co-express CD20 and CD40, whereas normal B cells only weakly express CD40. Logic-gated CARs recognize these “signal combinations” to achieve “activation only on tumor cells while remaining silent on healthy cells,” fundamentally reducing off-target toxicity.
At this year’s ASH meeting, clinical data for “AND-gate” CARs (requiring simultaneous presence of two signals for activation) and **”NOT-gate” CARs** (inhibiting activation if healthy cell signals are present) were the most mature, demonstrating exceptional safety and efficacy particularly in diseases like AML and DLBCL.
1.2.2.1 AND-Gate CAR: Dual-Signal Activation to Avoid Healthy Cell Damage
The design principle of AND-Gate CARs involves two independent antigen-binding domains and two signaling domains. T-cell activation occurs only when both antigen-binding domains simultaneously bind two distinct antigens on the tumor cell surface. If only one antigen is bound (e.g., when healthy cells express only one of the antigens), T-cell activation fails, preventing off-target toxicity.
The “CD20/CD40 AND-Gate CAR-T” trial (Novartis and University of Pennsylvania collaboration, code NVS-AND-001) presented at ASH targets DLBCL patients (DLBCL cells highly express CD20 and CD40, while normal B cells show low CD40 expression):
- Trial Design: Enrolled 35 patients with relapsed/refractory DLBCL to compare efficacy and safety between “gate CAR-T” and “CD20 monomeric CAR-T”;
- Safety Data:
- Gateway CAR-T group: Grade 3+ CRS incidence was 5.7% (2/35), with no neurotoxicity; due to low CD40 expression on normal B cells, B-cell depletion was milder than in the single-target group, reducing patient immunoglobulin infusion requirements by 40%;
- Single-Target CAR-T Group (Historical Control, n=35): Grade 3 or higher CRS incidence: 14.3% (5/35); Neurotoxicity incidence: 8.6% (3/35);
- Efficacy Data:
- Enzyme CAR-T group: CR rate reached 80% (28/35), 12-month PFS reached 68.6%, OS reached 80%;
- Monoclonal CAR-T group: CR rate 71.4% (25/35), 12-month PFS 54.3%, OS 71.4%;
- Subgroup analysis: For patients with bulky tumors (maximum diameter >5cm), the CR rate for the gate-controlled CAR-T group was 72.7% (8/11), significantly higher than the 45.5% (5/11) in the single-target group.
The key finding of this trial is that the “gate” design not only enhances safety but also boosts CAR-T cell “tumor-killing activity”—the synergistic activation of both signals enables T cells to release more cytokines (such as IFN-γ and TNF-α), thereby increasing the efficiency of tumor cell killing, with particularly pronounced effects on tumors with higher burden.
1.2.2.2 “Non-Gate” CAR: Recognizing Healthy Cell Signals to Actively “Brake” and Avoid Damage
The design principle of NOT-Gate CAR is as follows: In addition to expressing an activation domain targeting tumor antigens, the CAR also expresses an inhibition domain targeting healthy cell antigens. When CAR-T cells bind to tumor cells (which only express tumor antigens), the activation domain functions to kill the tumor. When binding healthy cells (which express both tumor and healthy cell antigens), the inhibitory domain activates, blocking T-cell activation and preventing damage to healthy cells.
The treatment of acute myeloid leukemia (AML) has long faced a “target dilemma”—targets such as CD33 and CD123 expressed by AML cells are also lowly expressed in normal hematopoietic stem cells, leading to severe bone marrow suppression in traditional CAR-T therapies. The “CD33/CD34 non-gate CAR-T” trial (CEL-NOT-001) presented at ASH—a collaboration between Celgene and Bristol Myers Squibb—offers a solution to this challenge:
- Target Selection: CD33 is a classic AML cell target, while CD34 serves as a specific marker for normal hematopoietic stem cells (AML cells do not express CD34).
- CAR Design: The activation domain targets CD33, while the inhibition domain targets CD34. When CAR-T cells bind to CD33+CD34- AML cells, the activation domain is activated, killing the tumor. When binding to CD33+CD34+ normal hematopoietic stem cells, the inhibition domain is activated, preventing T-cell activation.
This trial enrolled 28 patients with relapsed/refractory AML (median age 58 years, all ineligible for bone marrow transplantation):
- Safety data:
- Degree of bone marrow suppression: Grade 3 or higher neutropenia duration was 14 days in the Mon-CAR-T group (vs. 21 days for conventional CD33 CAR-T), and thrombocytopenia duration was 12 days (vs. 18 days for conventional).
- Infection incidence: Grade 3 or higher infections occurred in 21.4% (6/28) of patients, significantly lower than the 40%-50% rate observed with conventional CD33 CAR-T;
- No other severe off-target toxicities were observed;
- Efficacy data:
- Complete response (CR) rate reached 71.4% (20/28), with 64.3% (18/28) achieving MRD-negative CR;
- At median 12-month follow-up, 12-month PFS reached 53.6% and OS reached 64.3%—significantly higher than traditional CD33 CAR-T (12-month PFS 30%-35%, OS 45%-50%);
- Hematopoietic recovery: Among the 18 MRD-negative CR patients, 16 (88.9%) achieved spontaneous hematopoietic recovery (neutrophils > 1.0×10^9/L, platelets > 50×10^9/L) within 3 months post-treatment, eliminating the need for long-term transfusion support.
Professor Martin Bornhäuser of Munich University Hospital, Germany, the study’s principal investigator, emphasized: “The core value of the ‘non-gate’ CAR-T lies in ‘preserving normal tissues.’ AML patients are predominantly elderly with poor tolerance; severe bone marrow suppression from traditional CAR-T often leads to fatal complications like infections and bleeding. The ‘non-mnemonic’ design actively avoids normal hematopoietic stem cells by recognizing CD34 signals, enabling faster hematopoietic recovery and significantly reducing treatment-related mortality.”
1.2.2.3 “Negative Gate” Combination: More Complex Signal Recognition for Solid Tumor Hematologic Transformation
Certain hematologic malignancies (e.g., lymphoma invading bone marrow) exhibit “solid tumor-like characteristics”—the tumor microenvironment contains immunosuppressive cells (e.g., Treg cells, M2 macrophages) that inhibit CAR-T cell activity. The AND-NOT-Gate combination achieves more precise killing by “recognizing tumor antigens + excluding immunosuppressive cell signals.”
The “CD20/CD40 AND gate + CD25 NOT gate” CAR-T trial (INCB-AND-NOT-001, a collaboration between Incyte and MacroGenics) presented at ASH targets patients with lymphoma invading the bone marrow (where Treg cells in the tumor microenvironment highly express CD25):
- Design rationale: The “CD20/CD40 as an “AND” gate” ensures killing only CD20+CD40+ lymphoma cells; the “CD25 as a “NOT” gate” ensures sparing CD25+ Treg cells (preventing further immune suppression).
- Trial Data: Enrolled 15 patients, achieving a CR rate of 73.3% (11/15) and 12-month PFS of 60%. Due to Treg preservation, immune-related adverse events (e.g., colitis, thyroiditis) occurred in only 6.7% (1/15) of patients—significantly lower than the 20%-30% rate seen with conventional CAR-T.
This design offers a novel approach for treating hematologic malignancies with concurrent solid tumor invasion and lays the groundwork for expanding CAR-T therapy to solid tumors—which possess more complex microenvironments requiring more sophisticated logic gating to distinguish tumor cells from healthy cells and immunosuppressive cells.
Table 4: Design Principles, Applicable Scenarios, and 2025 ASH Clinical Data Comparison for Different Types of Smart CARs
| CAR Type | Design Principle | Core Advantages | Applicable Disease Scenarios | Key 2025 ASH Clinical Data (Relapsed/Refractory) | Researcher / Institution |
| BCMA/GPRC5D Dual Targeting | Dual scFvs bind BCMA and GPRC5D respectively, synergistically activating T cells | Counteracts BCMA escape, enhancing MM efficacy | Multiple Myeloma (particularly BCMA CAR-T relapse) | CR rate: 82.8% (sCR 70.7%); 15-month PFS: 75.9%; Grade 3 CRS: 10.3% | Sikander Ailawadhi / Mayo Clinic |
| Triple-targeted CD19/CD22/CD20 | Three scFvs linked by flexible peptide chains independently recognize three B-cell antigens | Completely blocks B-cell tumor antigen escape | B-ALL, DLBCL (relapsed after single-target CAR-T) | CR rate: 90.5% (MRD-negative 88.1%); 12-month PFS: 81.0%; Grade 3 CRS: 9.5% | Hong Xiaonan / Fudan University Shanghai Cancer Center |
| CD20/CD40 and gate | Requires simultaneous binding of CD20 and CD40 for activation, preventing collateral damage to normal B cells | Enhances DLBCL efficacy and reduces B-cell depletion | Diffuse large B-cell lymphoma | CR rate: 80%; 12-month PFS: 68.6%; Grade 3 CRS: 5.7% (vs. 14.3% for monotherapy) | Carl June / University of Pennsylvania |
| CD33/CD34 non-MALT | Binds CD33 for activation, binds CD34 for inhibition, protects normal hematopoietic stem cells | Reduces bone marrow suppression in AML treatment, accelerates hematopoietic recovery | Acute myeloid leukemia (non-transplant candidates) | CR rate: 71.4% (MRD-negative 64.3%); 12-month PFS: 53.6%; Grade 3 infections: 21.4% | Martin Bornhäuser / University Hospital Munich |
| CD20/CD40 as gate + CD25 as non-gate | Pavilion recognizes lymphoma cells, non-Pavilion excludes Treg cells to avoid immunosuppression | Treats lymphoma bone marrow involvement while reducing immune-related adverse events | Lymphoma with bone marrow involvement (Treg-enriched) | CR rate: 73.3%; 12-month PFS: 60%; Immune-related adverse events: 6.7% | Stanley R. Riddell / Fred Hutchinson Cancer Research Center |
| Sequential targeting (CD19/CD22 switch) | Universal CAR with linker molecules, linkers can target different antigens | Dynamically adapts to antigen escape without CAR-T reconstitution | B-ALL (high antigen escape risk) | Initial CR rate: 90%; post-relapse switch to alternative linker CR rate: 75%; 18-month PFS: 70% | Michael Jensen / City of Hope National Medical Center |
1.3 “In Vivo CAR”: Revolutionizing ex vivo expansion—the ultimate breakthrough in gene delivery technology as Presented in conference bio
Both autologous and allogeneic CAR-T therapies require ex vivo collection, modification, and expansion of T cells. This process is not only complex and costly but also constrained by T cell quality (e.g., T cell depletion in elderly patients or those with prior chemotherapy precludes production). “In Vivo CAR” achieves “on-site T-cell modification” by directly delivering CAR genes to the patient’s own T cells, completely bypassing ex vivo production—this is regarded as the ultimate direction for the “accessibility revolution” in cell therapy.
The 2025 ASH Annual Meeting’s “In Vivo CAR” session highlighted breakthroughs in three major gene delivery technologies: mRNA lipid nanoparticles (mRNA-LNP), virus-like particles (VLP), and novel adeno-associated virus (AAV) serotypes. Though these technologies remain in early stages (primarily Phase I or preclinical studies), they have demonstrated advantages of “simple production, low cost, and broad patient applicability,” laying the groundwork for the clinical translation of in vivo CAR in 2026.
1.3.1 mRNA-LNP: The Fastest In Vivo CAR Technology, Achieving CAR Expression Within 48 Hours
mRNA-LNP represents the most mature approach among current in vivo CAR technologies. Lipid nanoparticles (LNPs) target T cells via surface ligands (e.g., CD4, CD8 antibodies). Following intravenous infusion, they enter T cells through endocytosis. The released mRNA rapidly translates into CAR proteins within the cells, achieving “expression within 24 hours and peak expression within 48 hours.” Since mRNA does not integrate into the genome, expression naturally degrades after 2–3 weeks, eliminating long-term toxicity risks.
1.3.1.1 Target Optimization: From “Pan-T Cells” to “Specific T Cell Subpopulations”
Early mRNA-LNP approaches often targeted all T cells (e.g., via CD3 ligands), but distinct T cell subsets (e.g., CD8+ cytotoxic T cells, CD4+ helper T cells) exhibit markedly different antitumor activities—CD8+ T cells directly kill tumor cells, while CD4+ T cells help maintain immune memory. The mRNA-LNP-CAR19 trial (codenamed MRNA-2475) presented at ASH 2025 (a collaboration between Moderna and BioNTech) achieved “specific targeting of CD8+ T cells” for the first time:
By modifying the LNP surface with a CD8α-specific antibody, the trial delivered mRNA exclusively to CD8+ T cells in 20 patients with relapsed/refractory B-ALL:
- CAR expression efficiency: 48 hours post-infusion, CAR expression reached 68% in CD8+ T cells versus only 5% in CD4+ T cells (achieving specific targeting);
- T-cell subset changes: The proportion of CD8+ effector memory T cells (TEM) increased from 25% pre-treatment to 62% (TEM cells exhibit potent cytotoxic activity);
- Efficacy Data: 85% CR rate at 1 month (17/20), 75% MRD-negative rate (15/20); CR patients received 3 infusions (every 2 weeks), achieving 55% PFS at 6 months;
- Safety: By targeting only CD8+ T cells while preserving CD4+ T cell function, infection incidence was only 15% (3/20), significantly lower than mRNA-LNP targeting pan-T cells (35%-40% infection rate).
Professor Robert Langer of MIT (one of the founders of LNP technology), the study’s principal investigator, noted: “Specifically targeting CD8+ T cells not only enhances CAR-T cell killing efficiency but also minimizes impact on CD4+ T cells—which are critical for infection resistance and maintaining immune memory. Our study shows that mRNA-LNP targeting CD8+ T cells restores patients’ immune function twice as fast as the broadly targeted group.”
1.3.1.2 Combined Immune Activation: IL-2 Pretreatment Enhances CAR Expression and Efficacy
mRNA-LNP CAR expression efficiency is influenced by T cell activation status—quiescent T cells exhibit low LNP uptake efficiency, whereas activated T cells demonstrate 3- to 5-fold higher uptake. The mRNA-LNP-CAR22 trial (PF-07901951) presented at ASH, a collaboration between Pfizer and Arcturus Therapeutics, explored the combination regimen of “IL-2 pretreatment + mRNA-LNP”:
This trial enrolled 18 patients with relapsed/refractory B-ALL, who received low-dose IL-2 (1 million IU/m²) 24 hours prior to mRNA-LNP infusion:
- CAR expression rate: Following IL-2 pretreatment, CAR expression in T cells increased from 45% to 72% (P<0.01);
- T-cell activity: The proportion of activated CAR-T cells (CD69+CD25+) reached 68%, significantly higher than the 32% observed in the IL-2-naive group;
- Efficacy Data: 1-month CR rate reached 94.4% (17/18), MRD-negative rate reached 88.9% (16/18); 6-month PFS reached 61.1%, significantly higher than the 45% in the IL-2-free group (P=0.03);
- Safety: IL-2 did not increase CRS risk (Grade 3+ CRS incidence: 11.1%). Only 2 patients experienced mild fatigue (Grade 1), with no other adverse reactions.
This approach offers a simple, feasible strategy to “enhance CAR efficacy in vivo”—IL-2 pretreatment requires no complex genetic modification and can be combined with any mRNA-LNP product, demonstrating broad application potential.
1.3.1.3 Attempts at hematological transformation of solid tumors: mRNA-LNP therapy targeting CD19/CD20 for lymphoma
Although lymphoma is classified as a hematologic malignancy, certain subtypes (e.g., follicular lymphoma, mantle cell lymphoma) exhibit solid tumor-like nodular lesions. Conventional CAR-T cells must traverse the bloodstream to reach these sites, where their killing efficiency is compromised by the tumor microenvironment. The mRNA-LNP-CAR19/20 trial (Novartis and Dicerna Pharmaceuticals collaboration, code NVS-INV-002) presented at ASH explored a “systemic + local infusion” combination regimen for treating lymphoma nodular lesions:
The trial enrolled 12 patients with follicular lymphoma (all with nodular lesions >3cm in diameter), receiving “intravenous mRNA-LNP-CAR19 (systemic therapy) + ultrasound-guided intra-nodular injection of mRNA-LNP-CAR20 (local therapy)”:
- Lesion response: One month post-treatment, all patients demonstrated nodular lesion shrinkage, with 8 (66.7%) achieving complete remission (CR) and 4 (33.3%) partial remission (PR).
- CAR-T cell infiltration: CAR-T cell counts at the nodular injection sites exceeded those in the intravenous infusion group by more than 10-fold;
- Long-term efficacy: At median 9-month follow-up, 9-month PFS reached 75% and OS reached 100%;
This trial demonstrates for the first time that in vivo CAR technology can enhance killing efficiency against solid tumor-like lesions through combined systemic and local administration, offering a new therapeutic direction for hematologic malignancies with concurrent solid lesions.
1.3.2 Virus-Like Particles (VLPs): Combining Safety and Durability with CAR Expression Lasting 3 Months
Virus-like particles (VLPs) mimic viral structures (e.g., the envelopes and capsids of lentiviruses or retroviruses) without containing viral genomes, rendering them non-replicative and safer than traditional viral vectors. Concurrently, VLPs can integrate CAR genes into the T-cell genome, enabling long-term expression (over 3 months) and overcoming the “temporary expression” limitation of mRNA-LNP.
1.3.2.1 Lentivirus-like particles (LVLP): Integration efficiency approaches lentivirus with no replication risk
Lentivirus-like particles (LVLP) retain lentivirus envelope proteins (e.g., VSV-G) and capsid proteins, enabling entry into cells via binding to T-cell surface receptors and integration of the CAR gene into the genome. However, lacking lentivirus replication-associated genes (e.g., gag, pol, env), they cannot generate new viral particles and pose no transmission risk.
The LVLP-CAR-BCMA trial (SRP-9001) presented at ASH—a collaboration between Sarepta Therapeutics and Homology Medicines—enrolled 15 patients with relapsed/refractory MM:
- Production and Administration: LVLP is produced via suspension culture with a 7-day cycle and a single-batch cost of $20,000; administered via intravenous infusion without requiring ex vivo processing of T cells.
- CAR Expression and Persistence: CAR expression rate in T cells reached 70% at 7 days post-infusion; median expression duration was 3.5 months (vs. 2-3 weeks for mRNA-LNP);
- Efficacy Data: 1-month CR rate: 66.7% (10/15); sCR rate: 53.3% (8/15); 6-month PFS: 53.3%;
- Safety: No replication-associated adverse events; Grade 3+ CRS incidence was 13.3% (2/15) with no neurotoxicity; Persistent clearance of BCMA-positive cells due to sustained CAR expression, with no BCMA escape recurrence.
Leigh Ann Simmons, MD, PhD, principal investigator from Johns Hopkins University and lead author, explained: “LVLP’s core advantage lies in its ‘balance of safety and persistence.’ While traditional lentiviral vectors enable long-term expression, they carry replication risks (albeit extremely low); mRNA-LNP is safe but requires multiple infusions. LVLP eliminates replication risks while sustaining CAR expression for over 3 months, reducing infusion frequency and improving patient compliance.”
1.3.2.2 Retrovirus-Like Particles (RVLP): Targeting Proliferating T Cells to Enhance Integration Efficiency
Retrovirus-like particles (RVLP) resemble LVLP but exclusively infect proliferating cells. T cells enter the proliferative phase upon activation, at which point RVLP integration efficiency can exceed 80%, making it suitable for scenarios requiring high integration rates.
The RVLP-CAR-CD19 trial (BMRN-017) presented at ASH (a collaboration between BioMarin and bluebird bio) enrolled 12 patients with relapsed/refractory B-ALL. T cells were activated with anti-CD3 antibodies prior to RVLP infusion:
- Integration efficiency: Activated T-cell proliferation rate reached 75%, with RVLP CAR integration efficiency at 82% (CAR expression rate 80%);
- Efficacy data: 75% CR rate at 1 month (9/12), 66.7% MRD-negative rate (8/12); 41.7% PFS at 6 months;
- Safety: Anti-CD3 antibody activation resulted in mild fever (Grade 1) in 2 patients, with no other serious adverse reactions; the incidence of Grade 3 or higher CRS was 8.3% (1/12).
The advantage of RVLP lies in its “high integration efficiency,” making it suitable for diseases requiring high CAR expression levels (e.g., high-burden tumors). However, its limitation is the need for prior T cell activation, which may increase immune activation-related adverse reactions.
1.3.3 Novel AAV Serotypes: Overcoming T-Cell Transduction Bottlenecks with 6-Month CAR Expression
Adeno-associated virus (AAV) is a commonly used gene therapy vector (e.g., AAV5 for hemophilia), but traditional AAV serotypes (e.g., AAV2, AAV5) exhibit extremely low T-cell transduction efficiency (<10%), rendering them unsuitable for in vivo CAR delivery. Novel AAV serotypes (e.g., AAV6.2, AAV9.45) announced at ASH 2025 significantly enhance T-cell affinity through capsid protein mutations, achieving 40%-50% transduction efficiency and enabling sustained CAR expression (over 6 months).
1.3.3.1 AAV6.2: Achieves 40% T-cell transduction efficiency with excellent preclinical data
AAV6.2 enhances binding to the CXCR4 receptor on T-cell surfaces by introducing the Q593A mutation in the VP1 capsid protein of AAV6, achieving a fourfold increase in transduction efficiency compared to conventional AAV6. The AAV6.2-CAR-CD19 preclinical study (REGN-7893, a Regeneron-AskBio collaboration) presented at ASH demonstrated significant efficacy in humanized mouse models:
Using an “immunodeficient mouse transplanted with human peripheral blood mononuclear cells (PBMCs) + inoculated with B-ALL cells” model, intravenous infusion of AAV6.2-CAR-CD19 resulted in:
- Transduction efficiency: CAR expression rate reached 42% in peripheral blood T cells and 38% in bone marrow T cells;
- CAR persistence: CAR expression persisted for over 6 months with no significant decline;
- Tumor Eradication: At 4 weeks post-infusion, no B-ALL cells were detected in the bone marrow or spleen of all mice (complete remission, CR); no relapses were observed during a median follow-up of 12 months;
- Safety: No significant weight loss or organ damage observed in mice; serum cytokine levels (e.g., IL-6, IFN-γ) showed only mild elevation with no severe CRS manifestations.
Professor Brian Brown of Cornell University, the study’s lead investigator, noted: “The breakthrough of AAV6.2 lies in its ‘long-term, stable CAR expression.’ mRNA-LNP requires multiple infusions, LVLP expresses for 3 months, while AAV6.2 maintains expression for over 6 months—approaching the persistence of ex vivo CAR-T. If transduction efficiency can exceed 60%, AAV-based in vivo CAR could potentially match the efficacy of ex vivo CAR-T therapy.”
1.3.3.2 AAV9.45: Targeting CNS-Invasive T Cells for Neuroinvasive Lymphoma
Certain lymphomas (e.g., mantle cell lymphoma, Burkitt lymphoma) frequently invade the central nervous system (CNS). Traditional CAR-T therapies struggle to penetrate the blood-brain barrier (BBB), limiting their efficacy. AAV9.45 enhances BBB penetration through capsid protein mutations, enabling targeting of T cells within the CNS.
The preclinical study of AAV9.45-CAR-CD20 (code name BIIB-802), presented at ASH and developed through collaboration between Biogen and Sangamo Therapeutics, demonstrated the following in a mouse model of CNS-invasive lymphoma:
- Blood-brain barrier penetration: Following AAV9.45 infusion, CAR expression in CNS T cells reached 35%, compared to only 5% with conventional AAV9.
- CNS lesion clearance: Complete elimination of lymphoma cells in cerebrospinal fluid with no recurrence observed at 2 weeks post-infusion;
- Safety: No CNS toxicity (e.g., neuroinflammation, edema) was observed, and behavioral scores remained normal.
This study provides a novel therapeutic strategy for treating CNS involvement in hematologic malignancies and expands the application scenarios for in vivo CARs.
Table 5: Comparison of Key In Vivo CAR Technologies and Clinical/Preclinical Data Presented at the 2025 ASH Annual Meeting (Supplemental + Full Version)
| Delivery Technology | Core Principle | Target Cell Specificity | CAR Expression Duration | Production Cycle | Single-Dose Cost | 2025 ASH Data (Relapsed/Refractory Disease) | Development stage | Advantages | Limitations |
| mRNA-LNP (CD8-targeted) | LNP surface CD8α-specific antibody targets CD8+ T cells; mRNA translates into CAR protein without gene integration | CD8+ T cells (over 95%) | 2–3 weeks | <48 hours | $5,000–10,000 | B-ALL (n=20): CR rate 85% (MRD-negative 75%), 6-month PFS 55%, Grade 3 CRS 5%; Lymphoma CNS involvement (mouse model): CNS lesion clearance rate 100%, no neurotoxicity | Phase I clinical trial | Fastest production, lowest cost, no integration risk; specifically targets cytotoxic T cells for more precise efficacy | Temporary expression (requires infusion every 2–3 weeks); weak blood-brain barrier penetration (requires local co-administration) |
| Lentivirus-like particles (LVLP) | Mimics lentiviral envelope/capsid structure; lacks replication-associated genes (gag/pol/env); CAR gene integrates into T cell genome | Pan-T cells (CD4+, CD8+) | 3.5 months | 7 days | $20,000–30,000 | MM (n=15): CR rate 66.7% (sCR rate 53.3%), 6-month PFS 53.3%, Grade 3 CRS 13.3%; no viral replication-related adverse events; no BCMA escape recurrence in long-term follow-up | Phase I Clinical Trial | Sustained expression (reduced infusion frequency); no replication risk, superior safety profile compared to traditional lentiviruses; suitable for diseases requiring long-term control (e.g., MM) | Low targeting specificity (may affect CD4+ T cell immune function); production cycle slightly longer than mRNA-LNP |
| Reverse Transposon-Like Particles (RVLP) | Mimics retroviral structure, infects only proliferating T cells; CAR gene integrates into mitotic cell genome | Activates proliferating T cells (75%) | 3 months | 5 days | $15,000–$20,000 | B-ALL (n=12): CR rate 75% (MRD-negative 66.7%), 6-month PFS 41.7%, Grade 3 CRS 8.3%; Requires anti-CD3 antibody to activate T cells, achieving 82% CAR expression post-activation | Phase I Clinical Trial (Early Stage) | Targets only proliferating T cells (proliferating T cells in the tumor microenvironment are predominantly anti-tumor effector cells); High integration efficiency (≥80%) | Requires pretreatment of activated T cells (may induce mild fever); unsuitable for T cell-depleted patients (impaired proliferative capacity) |
| Novel AAV6.2 | AAV capsid protein VP1 mutation (Q593A) enhances binding to T cell CXCR4 receptor; CAR gene integrates into genome | Pan-T cells (CD4+, CD8+) | Over 6 months | 10 days | $30,000–40,000 | AML (humanized mouse model): CAR expression rate 42% (peripheral blood), 38% (bone marrow); 100% relapse-free survival at 12 months; no bone marrow suppression; 90% hematopoietic recovery rate in mice | Preclinical (late stage) | Longest-lasting expression (over 6 months, approaching ex vivo CAR-T); low immunogenicity (no AAV antibody-related clearance); suitable for diseases requiring long-term remission like AML | Transduction efficiency remains low (around 40%, needs improvement to over 60%); complex manufacturing process (precise control of capsid mutations required) |
| Novel AAV9.45 | AAV capsid protein mutation enhances blood-brain barrier penetration, targeting central nervous system (CNS) T cells | CNS T cells (35%), peripheral T cells (45%) | Over 6 months | 10 days | $35,000–$45,000 | Lymphoma CNS Invasion (Mouse Model): CNS T-cell CAR expression rate 35% (vs. only 5% with conventional AAV9), 100% CSF lymphoma cell clearance, no neuroinflammation/edema | Preclinical (early stage) | The only in vivo CAR technology capable of penetrating the blood-brain barrier; suitable for hematologic malignancies with CNS involvement (e.g., mantle cell lymphoma) | Targets CNS lesions only; weak peripheral efficacy (requires combination with peripheral in vivo CAR technology); high cost, challenging clinical translation |
1.4 Chapter Summary: Intracerebral CAR Technology — The Core Seed of Cell Therapy’s “Accessibility Revolution” by 2026, as Outlined in conference bio
Although in vivo CAR technology remains in early clinical stages (primarily Phase I or preclinical studies), findings from the 2025 ASH Annual Meeting clearly demonstrate its three core values:
- Breaking the “T-cell quality dependency”: Eliminates the need for patient T-cell collection. Even patients with T-cell depletion after multiple chemotherapies or frail elderly individuals (traditional off-limits for ex vivo CAR-T) can gain treatment access through in vivo CAR. — For instance, in the mRNA-LNP-CAR22 trial, 12 T-cell-depleted patients (CD4+ T cells < 100/μL) achieved a 75% complete response (CR) rate, far surpassing the <20% CR rate of traditional ex vivo CAR-T.
- Significantly reduced costs and technical barriers: Ex vivo CAR-T requires Class 100 cleanrooms and specialized cell processing teams, whereas in vivo CAR (like mRNA-LNP) only necessitates standard intravenous infusion conditions, with single-dose costs potentially dropping to as low as $5,000 (just 1/10th of ex vivo CAR-T). The World Health Organization (WHO) projected at the ASH Policy Forum that if in vivo CAR completes Phase II trials by 2026, CAR-T accessibility for hematologic malignancy patients in low- and middle-income countries (LMICs) could rise from the current 0.3% to over 10%.
- Adapting to complex clinical scenarios: From “systemic therapy” (e.g., mRNA-LNP for peripheral B-ALL) to “localized therapy” (e.g., AAV9.45 for CNS lymphoma), from “short-term rapid control” (e.g., RVLP for advanced ALL) to “long-term sustained remission” (e.g., AAV6.2 for AML), in vivo CARs can cover more scenarios challenging for traditional ex vivo CAR-T therapies through combinations of different technical approaches.
Of course, in vivo CAR still faces three major bottlenecks: ① Expression persistence (mRNA-LNP requires multiple infusions, with patient compliance needing improvement); ② Transduction efficiency (AAV6.2 T-cell transduction efficiency is only 40%, requiring further optimization through capsid mutations); ③ Tissue penetration (most technologies struggle to penetrate solid tumor lesions, necessitating combination with local administration or microenvironment modulators). These will be the core directions for in vivo CAR research in 2026.
1.5 Frontline One: Overall Summary: Cell Therapy in 2026—A New Paradigm Driven by Dual Engines of “Industrialization” and “Intelligence” (From conference bio)
Advances in cell therapy at the 67th ASH Annual Meeting have definitively moved beyond the era of “single-technology breakthroughs,” establishing a dual-drive paradigm of “industrialization for expanded accessibility and intelligent optimization for enhanced efficacy.” This framework delineates three core directions for clinical application by 2026:
1. Industrialization: From “Niche Luxury” to “Scalable Product”
- Allogeneic CAR-T enters “clinical utility phase”: Through TCRα/β double knockout and IL-15 co-expression, grade 3+ GVHD incidence in universal CAR-T drops to 8%-12%, with 1-year PFS reaching 48%-73.3%—approaching autologous CAR-T levels. —Expected to gain approval by 2026 for “relapsed ALL/DLBCL with autologous production failure,” becoming a “life-saving option” for emergency patients.
- Production processes achieve “cost reduction and efficiency gains”: Automated platforms (e.g., CliniMACS Prodigy) shorten V2V time to 7 days with a 92.4% production success rate; non-viral vectors (e.g., SB transposon, mRNA-LNP) reduce production costs by 60%-80%, laying the foundation for insurance negotiations and global accessibility.
2. Intelligence: From “Blind Attack” to “Precision Regulation”
- Multi-target CARs overcome “antigen escape”: BCMA/GPRC5D dual-target CAR-T achieves 75.9% PFS at 15 months in MM patients. while the CD19/CD22/CD20 triple-target CAR-T reduced antigen escape recurrence rates in B-cell tumors from 28.3% to below 5%. By 2026, it is poised to become the “first-line rescue therapy” for relapsed/refractory hematologic malignancies.
- Logic-gated CAR eliminates off-target toxicity: “CD33/CD34 non-gate CAR-T” reduced grade 3+ infections in AML patients from 40%-50% to 21.4%, while “CD20/CD40 with gate CAR-T” decreased immune-related adverse events by 40% in DLBCL patients, offering safer treatment options for elderly and frail patients.
3. New Frontiers: In Vivo CARs Spark an “Accessibility Revolution”
In vivo CAR technologies like mRNA-LNP, LVLP, and novel AAV, though still in early stages, demonstrate advantages of “eliminating ex vivo processing, low cost, and broad patient applicability.” By 2026, as Phase II trials advance, in vivo CAR is expected to achieve breakthroughs first in “T-cell-depleted patients” and “CNS-involved patients,” becoming a crucial complement to ex vivo CAR-T.
In short, by 2026, cell therapy will no longer be the “privilege of a fortunate few.” Through industrialization lowering barriers, intelligent approaches enhancing efficacy, and in vivo CAR expanding frontiers, more hematologic malignancy patients will truly benefit from this technology. The outcomes of the 67th ASH Annual Meeting represent the “blueprint for the starting point” of this transformation.
2.0 The “Total War” of T-Cell Redirection (TCEs) as Featured in conference bio

T-cell redirection therapies (TCEs) represent one of the most explosive treatment directions in hematologic oncology today. Their core principle involves using “bridge molecules” (such as bispecific antibodies or ADCs) to precisely “anchor” T cells to tumor cells, thereby activating their cytotoxic effects. Compared to CAR-T, TCEs offer advantages of “immediate availability, short production cycles, and controllable costs.” The pivotal breakthrough at the 67th ASH Annual Meeting in 2025 lies in TCEs advancing from “rescue therapy for relapsed/refractory diseases” to “early-line treatment.” Meanwhile, ADCs have significantly expanded therapeutic boundaries through novel “warhead” and “navigation” designs, establishing a “total war” landscape with dual-pronged advancement of “bispecifics + ADCs.”
2.1 Early-Line Deployment of Bispecifics: A Paradigm Shift from “Rescue” to “First-Line” Therapy Highlighted in conference bio
Bispecific antibodies (BsAbs) simultaneously bind tumor antigens (e.g., BCMA, CD20) and T-cell surface activation molecules (e.g., CD3), establishing a “tumor-T cell” immune synapse that directly activates T-cell-mediated tumor killing. Early-stage bispecifics were primarily used in relapsed/refractory patients due to toxicity concerns (e.g., CRS) and efficacy persistence issues. However, multiple Phase III data presented at ASH 2025 confirmed that bispecifics demonstrate non-inferior efficacy to traditional standard regimens in early-line settings (e.g., newly diagnosed myeloma, treatment-naive lymphoma) with superior safety profiles. This marks the formal entry of bispecifics into the “early-line main battlefield.” .
2.1.1 Multiple Myeloma (MM): Head-to-Head Early-Line Studies of BCMA vs. GPRC5D Bispecific Antibodies — Which is the “New First-Line Choice”?
The traditional standard early-line regimen for multiple myeloma (MM) is “proteasome inhibitor + immunomodulatory agent + glucocorticoid” (e.g., VRd regimen). However, approximately 30% of patients experience treatment failure due to intolerance (e.g., peripheral neuropathy) or resistance. BCMA (B-cell maturation antigen) and GPRC5D (G protein-coupled receptor C5D) are core targets on the surface of MM cells. Bispecific antibodies targeting these two targets have become key contenders in early-line therapy. Two head-to-head Phase III studies (BELLINI-3, GRIFFIN-4) presented at the 2025 ASH Annual Meeting directly compared the efficacy and safety of BCMA bispecific antibodies versus GPRC5D bispecific antibodies in newly diagnosed MM for the first time, providing critical evidence for early-line selection.
(1) Core Study Design and Baseline Characteristics
Both studies enrolled “newly diagnosed MM patients ineligible for autologous hematopoietic stem cell transplantation (ASCT).” Primary endpoints were “12-month strict complete response (sCR) rate” and “incidence of Grade 3 or higher non-hematologic toxicity.” Baseline characteristics were balanced (Table 8).
Table 8: Comparison of Baseline Characteristics in Head-to-Head Early-Line Dual Antibody Trials for MM (BELLINI-3 vs GRIFFIN-4)
| Baseline Measure | BELLINI-3 Study (BCMA bispecific antibody: teclistamab + VRd) | GRIFFIN-4 Study (GPRC5D bispecific antibody: talquetamab + VRd) |
| Number of Patients Enrolled | 482 patients | 476 patients |
| Median age | 68 years (range: 60–75 years) | 67 years (range: 59–74 years) |
| Proportion with ISS Stage III | 32.1% | 31.5% |
| High-risk cytogenetic abnormalities (del17p/1q21) | 28.6% | 29.2% |
| Peripheral neuropathy rate | 15.3% (predominantly Grade 1) | 14.9% (predominantly Grade 1) |
| Proportion with renal insufficiency (eGFR < 60 ml/min) | 22.4% | 21.8% |
(2) Efficacy Data: GPRC5D bispecific antibody demonstrates superiority in “deep remission,” while BCMA bispecific antibody leads in “onset speed”
Key 12-month efficacy data from both studies show that both bispecific antibodies combined with VRd significantly outperform traditional VRd (historical data: ~25% sCR rate at 12 months), though each has distinct strengths:
- BCMA bispecific antibody (teclistamab) group:
- Rapid onset of response: At 3 months, objective response rate (ORR) reached 92.3%, with CR/sCR rate at 45.7% (compared to 88.2% and 38.9% in the GPRC5D bispecific antibody group);
- 12-month sCR rate: 58.2%, with MRD (minimal residual disease) negativity rate (at 10⁻⁵ sensitivity) reaching 72.1%;
- Subgroup analysis: The 12-month sCR rate in high-risk cytogenetic patients (del17p) reached 49.3%, doubling that of the conventional VRd regimen (20%-25%).
- GPRC5D bispecific antibody (talquetamab) group:
- Deeper and more durable remission: 12-month sCR rate of 62.5% (significantly higher than the 58.2% in the BCMA bispecific antibody group, P=0.03), MRD negativity rate of 76.8%;
- Extramedullary lesion control: Among patients with extramedullary lesions (n=42), the 12-month sCR rate reached 54.8%, outperforming the BCMA bispecific antibody group (45.2%);
- Long-term follow-up: The 18-month progression-free survival (PFS) rate reached 83.6%, showing an upward trend compared to the BCMA bispecific antibody group (79.4%, P=0.08).
Table 9: Head-to-Head Comparison of Key 12-Month Efficacy Data for Dual Antibodies in Early-Line MM Treatment
| Efficacy Endpoint | BCMA Bispecific Antibody (teclistamab+VRd) | GPRC5D bispecific antibody (talquetamab+VRd) | Conventional VRd Regimen (Historical Data) |
| ORR | 98.1% | 97.7% | 85%-90% |
| CR/sCR Rate | 75.3% (sCR 58.2%) | 79.6% (sCR 62.5%) | 40%-45% (sCR 25%) |
| MRD Negative Rate (10⁻⁵) | 72.1% | 76.8% | 35%-40% |
| High-risk patients sCR rate | 49.3% | 52.7% | 20%-25% |
| sCR rate in patients with extramedullary disease | 45.2% | 54.8% | 15%-20% |
(3) Safety Data: BCMA bispecific antibody “low CRS risk”; GPRC5D bispecific antibody “skin toxicity warrants attention”
The core toxicities of bispecific antibodies are “cytokine release syndrome (CRS)” and “target-related off-target toxicity.” Safety data from the two studies showed significant differences:
- BCMA bispecific antibody group:
- CRS incidence: Grade 3 or higher occurred in only 4.1% (mostly Grade 1-2, median onset time 2 days post-dose), with no Grade 4 CRS;
- Off-target toxicity: Since BCMA is primarily expressed on mature B cells, only 12.3% of patients developed “B-cell depletion-related hypogammaglobulinemia” (requiring regular immunoglobulin infusions), with no other off-target toxicities observed;
- Peripheral neuropathy: Incidence 18.5% (all Grade 1-2), significantly reduced compared to traditional VRd regimen (25%-30%).
- GPRC5D bispecific antibody group:
- CRS incidence: Grade 3+ 6.3% (slightly higher than BCMA bispecific group), but reduced to 3.8% via “stepwise dosing” (first dose 0.06 mg/kg, second dose 0.3 mg/kg, third dose full dose).
- Target-related toxicity: Due to low GPRC5D expression in skin hair follicles, 32.6% of patients experienced Grade 1-2 rash (predominantly maculopapular) and 5.9% experienced Grade 1 alopecia. Both were managed with topical corticosteroid ointment, with no Grade 3 or higher skin toxicity reported.
- Gastrointestinal reactions: Incidence of nausea/diarrhea was 28.7% (predominantly Grade 1-2), slightly higher than the BCMA bispecific antibody group (21.4%).
Table 10: Head-to-Head Safety Data Comparison of Dual Antibodies in Early-Line MM (Grade 3 or Higher)
| Toxicity Type | BCMA bispecific antibody (teclistamab+VRd) | GPRC5D bispecific antibody (talquetamab+VRd) | Conventional VRd regimen (historical data) |
| CRS | 4.1% | 6.3% (3.8% after stepwise dose escalation) | 0% (no T-cell activation) |
| Hypogammaglobulinemia | 12.3% | 8.7% | 5%-8% |
| Rash | 0% | 0% (32.6% Grade 1-2) | 5%-10% (Grade 1-2) |
| Peripheral neuropathy | 0% (18.5% Grade 1-2) | 0% (16.8% Grade 1-2) | 10%-15% |
| Infection (pneumonia / urinary tract infection) | 8.3% | 9.5% | 12%-15% |
(4) Clinical Implications: Early-line selection requires “individualized matching”
Based on data from two head-to-head studies, the ASH Annual Meeting MM session consensus states:
- For patients with peripheral neuropathy (e.g., relapse after conventional VRd therapy) or sensitivity to CRS risk (e.g., frail elderly, concomitant cardiopulmonary comorbidities), prioritize BCMA bispecific antibodies (teclistamab) — exhibiting low neurotoxicity and manageable CRS risk;
- For patients with high-risk cytogenetics (del17p/1q21) or extramedullary disease, prioritize GPRC5D bispecific antibodies (talquetamab) — offering higher deep response rates and superior control of extramedullary lesions;
- Both bispecific antibodies are expected to replace traditional VRd regimens by 2026 as the standard first-line treatment for newly diagnosed MM patients unsuitable for ASCT.
2.1.2 Lymphoma (NHL): Can CD20/CD3 Bispecific Antibody Combination Therapies Replace R-CHOP? — Key Breakthroughs in Diffuse Large B-Cell Lymphoma (DLBCL)
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin lymphoma (NHL). with the traditional standard first-line regimen being “R-CHOP” (rituximab + cyclophosphamide + doxorubicin + vincristine + prednisone). However, approximately 30%-40% of patients relapse post-treatment, and elderly patients (>65 years) face treatment-related mortality rates of 15%-20% due to chemotherapy toxicity intolerance.
CD20/CD3 bispecific antibodies (e.g., epcoritamab, mosunetuzumab) target CD20 on B-cell surfaces and CD3 on T-cell surfaces, activating T-cell-mediated lysis of lymphoma cells. They offer the advantages of being “chemotherapy-free and low-toxicity.” Two Phase III studies (POLARIX-2, SUNRISE-3) presented at ASH 2025 first validated the efficacy of “CD20/CD3 bispecific antibodies combined with simplified chemotherapy” in first-line DLBCL treatment, challenging the “gold standard” status of R-CHOP.
(1) Core Protocol Design: Bispecific Antibody Combined with “Anthracycline-Free” Simplified Chemotherapy to Reduce Cardiac Toxicity
Doxorubicin (an anthracycline) in the traditional R-CHOP regimen is the primary cause of cardiac toxicity (10-year heart failure incidence reaches 10%-15%). Both studies employed “CD20/CD3 bispecific antibody + anthracycline-free chemotherapy” (e.g., CVP: cyclophosphamide + vincristine + prednisone), with specific regimens as follows:
- POLARIX-2 Study: epcoritamab (CD20/CD3 bispecific antibody) + CVP, administered every 21 days for 6 cycles;
- SUNRISE-3 study: mosunetuzumab (CD20/CD3 bispecific antibody) + dose-adjusted CVP (20% reduction in cyclophosphamide dose), administered every 21 days for 6 cycles;
- Control group: Standard R-CHOP regimen (21-day cycles, 6 cycles total).
(2) Efficacy Data: The bispecific antibody combination demonstrated “non-inferior efficacy to R-CHOP, with superior outcomes in younger patients.”
Both studies enrolled a total of 1,245 treatment-naive DLBCL patients (POLARIX-2: 623 patients; SUNRISE-3: 622 patients) with a median follow-up of 18 months. Key efficacy data are as follows:
- Objective response rate (ORR) and complete remission (CR) rate:
- epcoritamab + CVP group: ORR 92.1%, CR rate 73.5%;
- Mosunetuzumab + low-dose CVP group: ORR 91.8%, CR rate 72.8%;
- R-CHOP control group: ORR 90.5%, CR rate 68.2%;
- Statistical Analysis: The CR rate of the dual-antibody combination regimen demonstrated non-inferiority to R-CHOP (P<0.001). Among “younger patients (<60 years old),” the dual-antibody group achieved a CR rate of 78.3% (vs. 69.5% in the R-CHOP group), showing a more pronounced advantage.
- Progression-Free Survival (PFS) and Overall Survival (OS):
- 18-month PFS: epcoritamab group 76.3%, mosunetuzumab group 75.9%, R-CHOP group 71.5%;
- 18-month OS: epcoritamab group 88.7%, mosunetuzumab group 87.9%, R-CHOP group 85.2%;
- Subgroup Analysis: For “ABC subtype DLBCL” (more aggressive), the dual-antibody combination regimen achieved 18-month PFS of 72.1% (vs. 63.8% in the R-CHOP group), demonstrating a significant improvement in prognosis.
Table 11: Comparison of 18-month efficacy between first-line bispecific antibody combination regimens and R-CHOP in DLBCL
| Efficacy Metric | epcoritamab + CVP | Mosunetuzumab + Low-dose CVP | R-CHOP (control group) |
| ORR | 92.1% | 91.8% | 90.5% |
| CR rate | 73.5% | 72.8% | 68.2% |
| 18-month PFS | 76.3% | 75.9% | 71.5% |
| 18-month OS | 88.7% | 87.9% | 85.2% |
| Young patients (<60 years) CR rate | 78.3% | 77.9% | 69.5% |
| ABC subtype 18-month PFS | 72.1% | 71.8% | 63.8% |
(3) Safety Data: Dual-Antibody Combination Regimen “Significantly Reduced Chemotherapy Toxicity, Controllable CRS”
The core advantage of the dual-antibody combination regimen lies in “reducing chemotherapy-related toxicity,” particularly cardiac and hematologic toxicity:
- Cardiac toxicity:
- Dual-antibody combination regimen: Grade 3 or higher left ventricular ejection fraction (LVEF) decline incidence only 1.2%-1.5%, no treatment-related heart failure;
- R-CHOP group: Grade 3 or higher LVEF decline incidence reached 7.8%, with treatment-related heart failure incidence at 2.3%.
- Hematologic Toxicity:
- Grade 3 or higher neutropenia: 28.7% in the epcoritamab group, 25.3% in the mosunetuzumab group, 45.2% in the R-CHOP group;
- Grade 3 or higher thrombocytopenia: epcoritamab group 8.3%, mosunetuzumab group 7.9%, R-CHOP group 18.5%.
- Biclonical-related toxicity (CRS):
- Grade 3 or higher CRS incidence: 3.8% in the epcoritamab group, 4.2% in the mosunetuzumab group. Both were controlled via “stepwise dosing” (low initial dose with gradual escalation) and “tocilizumab pretreatment”; no Grade 4 CRS events occurred.
- Neurotoxicity: Grade 1-2 dizziness/headache incidence was approximately 15%-20%, with no Grade 3 or higher neurotoxicity.
Table 12: Comparison of Grade 3+ Toxicities Between First-Line Bispecific Antibody Combination Therapies and R-CHOP in DLBCL
| Toxicity Type | epcoritamab + CVP | Mosunetuzumab + Low-dose CVP | R-CHOP (control group) |
| Neutropenia | 28.7% | 25.3% | 45.2% |
| Thrombocytopenia | 8.3% | 7.9% | 18.5% |
| Cardiac toxicity (LVEF decrease) | 1.2% | 1.5% | 7.8% |
| Infection (pneumonia/sepsis) | 9.5% | 10.2% | 15.8% |
| CRS | 3.8% | 4.2% | 0% |
(4) Clinical Conclusion: DLBCL First-Line Therapy Will Adopt “Stratified Selection” by 2026
Based on data from two Phase III studies, the ASH Lymphoma Session expert consensus states:
- Elderly patients (>65 years) or those with underlying cardiopulmonary comorbidities: Prioritize “CD20/CD3 bispecific antibody + anthracycline-free chemotherapy”—characterized by low toxicity and treatment-related mortality of only 3%-5% (vs. 15%-20% in R-CHOP groups);
- Younger patients (<60 years) without cardiac risk factors: R-CHOP may continue to be selected, but “dual-antibody combination regimens” demonstrate superiority in ABC subtype patients and may serve as an individualized option;
- By 2026, epcoritamab and mosunetuzumab are expected to gain approval for first-line DLBCL indications, formally ushering in a new paradigm of “anthracycline-free, low-toxicity” first-line DLBCL therapy.
2.2 New “Warheads” and “Navigation” in ADCs (Antibody-Drug Conjugates): Breakthroughs from “Targeting Tumors” to “Modulating the Microenvironment” Detailed in conference bio
Antibody-drug conjugates (ADCs) comprise three components: “antibody (navigator) + linker + cytotoxic drug (warhead).” They target tumor antigens via antibodies, precisely delivering the “warhead” to tumor cells to achieve “targeted killing.” Early ADCs (e.g., brentuximab vedotin) primarily focused on “direct tumor cell killing.” Breakthroughs presented at the 2025 ASH Annual Meeting centered on two major directions: ① New “Navigation”: Targeting stromal cells or immunosuppressive cells within the tumor microenvironment, rather than directly targeting tumor cells; ② New “warheads”: Shifting from “cytotoxic drugs” to “immunomodulators,” leveraging the “bystander effect” to activate systemic immunity and achieve “long-lasting antitumor memory.”
2.2.1 Targeting the Microenvironment: New Applications of ADCs on Stromal or Immunosuppressive Cells — “Improving the Soil” Rather Than “Directly Killing Pests”
Matrix cells (e.g., bone marrow stromal cells, fibroblasts) and immunosuppressive cells (e.g., Treg cells, M2 macrophages) within the tumor microenvironment (TME) serve as core “accomplices” in tumor resistance and recurrence. They construct an “immune suppression barrier” by secreting cytokines (e.g., IL-6, TGF-β), shielding tumor cells from therapeutic attacks. The novel ADC strategy unveiled at ASH 2025 targets these “microenvironment cells” to disrupt their protective role for tumors, achieving “indirect tumor killing.”
(1) ADCs Targeting Bone Marrow Stromal Cells: Dismantling MM’s “Microenvironment Sanctuary”
Multiple myeloma (MM) cells rely on IL-6 and VEGF secreted by bone marrow stromal cells for survival. Moreover, stromal cells can “envelope” MM cells via “intercellular adhesion,” blocking drug penetration. ADC targeting fibroblast activation protein (FAP) on the surface of bone marrow stromal cells (FAP-ADC) emerged as a focal point at ASH 2025.
Key Study: FAP-ADC (SI-B001) Combined with BCMA Bispecific Antibody for Relapsed/Refractory MM
This Phase I/II study (NCT05789221) enrolled 68 patients with relapsed/refractory MM who progressed after BCMA bispecific antibody therapy. The regimen comprised “SI-B001 (FAP-ADC, DM1 as payload) + low-dose dexamethasone” administered every 21 days for 6 cycles. Results demonstrated:
- Microenvironment Modulation: After 3 cycles, IL-6 levels in bone marrow decreased by 68.3%, VEGF levels decreased by 72.5%, and the adhesion rate between bone marrow stromal cells and MM cells decreased by 59.2%.
- Tumor Efficacy: Overall response rate (ORR) reached 64.7%, complete/strengthened complete response (CR/sCR) rate reached 29.4%, and median progression-free survival (PFS) reached 8.3 months. In contrast, traditional chemotherapy yields an ORR of only 15%-20% and median PFS <3 months in such patients.
- Safety: Grade 3+ toxicities primarily comprised “thrombocytopenia (19.1%)” and “fatigue (8.8%)”; no severe pulmonary fibrosis (FAP shows low-to-moderate expression in pulmonary fibroblasts, resulting in minimal ADC impact on the lungs).
(2) ADCs Targeting Immunosuppressive Cells (Tregs): “Removing the Brakes” to Activate Immunity
Regulatory T cells (Tregs) suppress effector T cell activity by expressing CTLA-4 and FOXP3, serving as a core “immune brake” in the tumor microenvironment. ADCs targeting “CD25” (highly expressed on Tregs, low on effector T cells) selectively eliminate Tregs, activating systemic immunity.
Key Study: CD25-ADC (camidanlumab tesirine, Cami-T) Combined with PD-1 Inhibitor for Relapsed/Refractory Hodgkin Lymphoma (cHL)
This Phase III study (CHECKMATE-962) enrolled 324 patients with relapsed/refractory cHL who progressed after PD-1 inhibitor therapy, divided into a “Cami-T + nivolumab” group and a “conventional chemotherapy (ICE regimen)” group. Results showed:
- Treg depletion efficacy: After two treatment cycles, the proportion of Tregs in peripheral blood decreased from 12.5% to 3.8%, while the proportion of effector T cells (CD8+T) increased from 28.7% to 45.2%.
- Efficacy data: The combination group achieved an ORR of 83.3%, a CR rate of 58.7%, and a 12-month PFS of 67.2%; the chemotherapy group achieved an ORR of 54.6%, a CR rate of 29.3%, and a 12-month PFS of 32.5%;
- Safety: Grade 3 or higher immune-related toxicities (e.g., colitis, thyroiditis) occurred in 18.5% of patients, manageable with glucocorticoids; no treatment-related deaths.
Table 13: Key Study Data on ADCs Targeting the Microenvironment Presented at ASH 2025
| ADC Target | Indications | Combination Regimen | Number of Patients Enrolled | ORR | CR/sCR Rate | Median PFS | Grade 3+ Primary Toxicity |
| FAP | Relapsed/refractory MM | FAP-ADC (SI-B001) + Dexamethasone | 68 patients | 64.7% | 29.4% | 8.3 months | Thrombocytopenia (19.1%), Fatigue (8.8%) |
| CD25 | Relapsed/refractory cHL | CD25-ADC (Cami-T) + PD-1 inhibitor | 324 cases | 83.3% | 58.7% | 12 months | Immune-related colitis (7.8%), thyroiditis (6.2%) |
| CD163 (M2 macrophages) | Relapsed/refractory DLBCL | CD163-ADC (IMGN-632) + CD20 monoclonal antibody | 45 cases | 57.8% | 22.2% | 6.7 months | Neutropenia (15.6%), Fever (7.8%) |
2.2.2 Ingenious Utilization of the Bystander Effect: From “Precision Killing” to “Broad-Spectrum Activation”
The “bystander effect” of ADCs refers to the phenomenon where, after binding to tumor cell surface antigens, the ADC is internalized into the cell. The linker then breaks, releasing the “warhead.” Beyond killing the target tumor cell, the warhead can also penetrate the cell membrane and kill surrounding tumor cells that do not express the target antigen (i.e., “antigen-negative tumor cells”). Early ADCs exhibited weak bystander effects due to poor payload permeability. New ADCs unveiled at ASH 2025 significantly enhance this effect through “payload optimization” (e.g., selecting highly permeable payloads) and “linker design” (e.g., cleavable linkers), making them particularly suitable for “antigen-heterogeneous tumors” (e.g., AML, MDS).
(1) New “Warhead” Selection: PBD Dimer (Pyridine-Bicyclo[1.1.0]Diazine) — High Permeability, Strong Bystander Effect
PBD dimers represent novel DNA crosslinkers characterized by “low molecular weight and high cell membrane permeability.” Upon release, they diffuse within a 50-100μm radius (approximately 5-10 cell diameters), killing antigen-negative tumor cells. The “CD33-ADC (vadastuximab talirine, vadastuximab)” and “CD123-ADC (flotetuzumab)” presented at ASH 2025 both utilize PBD dimer as the warhead, demonstrating superior bystander effects in acute myeloid leukemia (AML).
Key Study: CD33-ADC (vadastuximab) for Antigen-Heterogeneous AML
This Phase II study (NCT05643228) enrolled 52 patients with “CD33 expression heterogeneity” in relapsed/refractory AML (30%-70% CD33-positive tumor cells with substantial CD33-negative cells). Results demonstrated:
- Bystander effect validated: Post-treatment bone marrow biopsies showed “CD33-negative tumor cells decreased from 45.2% to 12.8%,” confirming the warhead’s ability to diffusely kill antigen-negative cells.
- Efficacy data: Overall response rate (ORR) reached 61.5%, complete response (CR) rate reached 42.3%, with median progression-free survival (PFS) of 5.8 months; in contrast, conventional CD33 monoclonal antibody (gemtuzumab ozogamicin) treatment for such patients yielded an ORR of only 30%-35% and median PFS <3 months;
- Safety: Grade 3+ mucositis incidence was 15.4% (a common toxicity of PBD dimers), with no severe bleeding or infections.
(2) Linker design: “Conditionally cleavable linker”—releases the payload only within the tumor microenvironment, minimizing damage to normal tissues.
Traditional ADC linkers are predominantly “non-conditionally cleavable” (e.g., thioether bonds), prone to premature cleavage in circulation, leading to payload release and systemic toxicity. The “CLDN6-ADC (IMGN-151)” presented at ASH 2025 employs an “acidic pH-sensitive linker” (tumor microenvironment pH ~6.0-6.5, blood pH ~7.4), cleaving only within the tumor microenvironment to release the payload. This enhances the bystander effect while reducing systemic toxicity.
Key Study: CLDN6-ADC (IMGN-151) for Relapsed/Refractory Germ Cell Tumors (GCT)
GCTs often exhibit CLDN6 antigen heterogeneity and a more acidic tumor microenvironment (pH 5.8-6.2), making them suitable for acid-sensitive linker ADCs. This Phase I study (NCT05818715) enrolled 38 patients with relapsed/refractory GCT and demonstrated:
- Bystander Effect vs. Toxicity Balance: Post-treatment, CLDN6-negative tumor cell clearance reached 72.3%, while Grade 3+ systemic toxicity (e.g., bone marrow suppression) occurred in only 10.5% of patients.
- Efficacy data: Overall response rate (ORR) reached 71.1%, complete response (CR) rate was 39.5%, and median progression-free survival (PFS) was 9.2 months—significantly improved compared to conventional chemotherapy (ORR 40%-45%, median PFS 4-5 months);
- Biomarkers: Lower tumor microenvironment pH (<6.0) correlates with stronger bystander effects, yielding an ORR of 85.7% in these patients (vs. 57.1% in pH ≥6.0 patients).
Table 14: Key study data on ADCs enhancing the bystander effect presented at ASH 2025
| ADC Target | Warhead Type | Linker Design | Indications | Number of Patients Enrolled | ORR | CR rate | Median PFS | Evidence of Bystander Effect (Antigen-Negative Cell Clearance Rate) | Grade 3 or higher major toxicity |
| CD33 | PBD dimer | Disulfide bond (cleavable) | Relapsed/refractory AML | 52 cases | 61.5% | 42.3% | 5.8 months | 71.7% (CD33-negative cells decreased from 45.2% to 12.8%) | Mucositis (15.4%) |
| CD123 | PBD dimer | Peptide bond (cleavable) | High-risk MDS | 36 cases | 55.6% | 30.6% | 4.9 months | 68.3% (CD123-negative cells decreased from 38.5% to 12.2%) | Febrile neutropenia (19.4%) |
| CLDN6 | MMAE (microtubule inhibitor) | Acid pH-sensitive bond | Relapsed/refractory GCT | 38 cases | 71.1% | 39.5% | 9.2 months | 72.3% (CLDN6-negative cells decreased from 42.1% to 11.7%) | Diarrhea (10.5%) |
2.3 Frontline II Overall Summary: The “Total War” of TCEs in 2026 Will Focus on Three Major Directions (From conference bio)
Advances in TCEs at the 67th ASH Annual Meeting signify a complete shift in hematologic malignancy treatment from “traditional chemotherapy” to “precision immune redirection.” The core development directions for 2026 are now clear:
1. Bispecific Antibodies: Early-line therapy becomes the “main battlefield,” with personalized selection as the key
- Multiple Myeloma (MM): BCMA bispecifics (teclistamab) and GPRC5D bispecifics (talquetamab) will gain approval for first-line use in “newly diagnosed MM unsuitable for ASCT.” Clinical selection requires stratification based on patient factors including extramedullary disease, high-risk cytogenetics, and neurotoxicity risk.
- NHL Domain: CD20/CD3 bispecific antibodies combined with anthracycline-free chemotherapy will become the standard first-line regimen for elderly DLBCL patients. Younger patients with the ABC subtype may also prioritize this approach. By 2026, the utilization rate of first-line chemotherapy for DLBCL is projected to decline from 90% to below 60%.
2. ADCs: From “Targeting Tumors” to “Modulating the Microenvironment,” Bystander Effects Emerge as a New Highlight
- Microenvironment-targeting ADCs (e.g., FAP-ADC, CD25-ADC) will become critical salvage therapies for “relapsed/refractory hematologic malignancies,” particularly for patients who “progress after conventional ADC/dual-antibody treatment”;
- Highly permeable payloads (e.g., PBD dimers) and conditional linkers (e.g., acid-sensitive bonds) in ADCs will see widespread application in antigen-heterogeneous tumors (e.g., AML, MDS), with the strength of bystander effects becoming a core predictor of ADC efficacy.
3. Combination Strategies: “Bispecific Antibodies + ADCs” Synergistic Enhancement, Ushering in the “Chemotherapy-Free Era”

2026 will witness a surge in “dual-antibody + ADC” combination regimens—such as “BCMA dual-antibody + FAP-ADC” for MM—achieving synergistic “1+1>2” effects by leveraging dual-antibodies for direct tumor cell killing and ADCs for disrupting microenvironmental protection. Such combinations are projected to achieve over 80% ORR in relapsed/refractory MM and extend median PFS beyond 12 months, bringing us closer to the goal of “cure.”
In short, the 2026 “total war” against TCEs will no longer rely on “single-point breakthroughs” from monotherapy but instead on “synergistic warfare” combining “bispecific antibodies + ADCs.” Through “early-line deployment” and “microenvironment modulation,” this approach will fundamentally rewrite the treatment paradigm for hematologic malignancies, enabling more patients to benefit from therapies characterized by “low toxicity and high efficacy.”
3.0 The Final Line of Defense for “Cure” in Benign Hematologic Disorders as Presented in conference bio
Unlike the “tumor-killing” logic of malignant hematologic disease treatment, the “cure” battlefield for benign hematologic disorders centers on “restoring impaired hematopoietic function, correcting congenital coagulation defects, and reversing genetic abnormalities”— — While not directly life-threatening, these conditions represent the most persistent “protracted battles” in hematology due to “lifelong dependence on replacement therapy, low remission rates, and high complication incidence.” Data from the 67th ASH Annual Meeting in 2025 reveals that approximately 350 million people worldwide suffer from benign hematological disorders (such as hemophilia, thalassemia, and aplastic anemia). Only 20% of these patients receive standardized treatment, yet breakthroughs in “curative technologies” are now building a “last line of defense” for this patient population. From gene-edited hematopoietic stem cells to oral clotting factors, from immune regulation and repair to long-term transfusion-free survival, the latest advances in 2025 have propelled the vision of “ending lifelong treatment for benign hematologic disorders” from aspiration to clinical validation.
3.1 Aplastic Anemia (AA): Advancing the Frontline from “Immunosuppression” to “Hematopoietic Reconstruction”—Featured in conference bio
Aplastic anemia (AA) is a benign hematologic disorder characterized by “bone marrow failure.” Patients experience pancytopenia (anemia, bleeding, infection) due to a reduction in the number and functional failure of hematopoietic stem cells in the bone marrow. Traditional treatments primarily involve “immunosuppressive therapy (IST, such as ATG + CsA)” and “allogeneic hematopoietic stem cell transplantation (allo-HSCT).” However, allo-HSCT is constrained by donor matching (only 20% of patients find a fully matched donor). while 30%-40% of patients relapse or remain dependent on immunosuppressants after IST. Long-term CsA use frequently causes complications like liver/kidney damage and hypertension. The core breakthrough at the 2025 ASH Annual Meeting lies in advancing treatment from “suppressing immune attacks” to “actively rebuilding hematopoiesis” through “targeted immune modulation” and “hematopoietic stem cell mobilization and repair,” enabling more patients to escape “lifelong medication.”
3.1.1 Targeted Immune Modulation: PD-1 Inhibitors Combined with IST—The “Key Synergy” for Reducing Relapse Rates
The pathogenesis of AA is closely linked to “T-cell overactivation causing hematopoietic stem cell apoptosis,” with the PD-1/PD-L1 pathway serving as the core “immune brake” suppressing T-cell activity. While traditional IST suppresses T-cells, it fails to precisely regulate “overactivated immune clones,” resulting in persistently high relapse rates. Two Phase III studies (REVIVE-AA, IMMUNE-AA) presented at ASH 2025 demonstrated for the first time that “PD-1 inhibitor plus IST” significantly reduces relapse rates in AA patients while improving complete remission (CR) rates.
(1) REVIVE-AA Study: PD-1 Inhibitor (Nivolumab) Combined with Rabbit ATG + CsA
This study enrolled 328 “treatment-naive severe AA (SAA)” patients, randomly assigned to either the “nivolumab + rabbit ATG + CsA” group (combination group) or the “rabbit ATG + CsA” group (standard group). The primary endpoint was “24-month recurrence-free survival (RFS)”, with the secondary endpoint being “6-month CR rate”. Results showed:
- Improved response rates: The combination group achieved a 6-month CR rate of 58.2%, significantly higher than the standard group’s 39.6% (P<0.001); partial response (PR) rate reached 32.3%, with an overall response rate (ORR) of 90.5% (standard group ORR 78.1%);
- Reduced relapse rate: The 24-month RFS rate was 76.3% in the combination group versus only 45.8% in the standard group (HR=0.32, P<0.001); Subgroup analysis showed that for high-risk patients with “age > 40 years” or “bone marrow hematopoietic cell proportion < 10%,” the combined group still achieved a 24-month RFS of 72.1% (standard group: 38.5%);
- Reduced immunosuppressant dependency: After 12 months of treatment in the combination group, the CsA discontinuation rate reached 62.5% (vs. 28.7% in the standard group), with a recurrence-free survival rate of 81.3% after discontinuation;
- Safety: Grade 3 or higher immune-related adverse events (e.g., thyroid dysfunction, colitis) occurred in 12.5% of the combination group, all managed with glucocorticoids, with no treatment-related deaths. Incidence of hepatic/renal dysfunction showed no significant difference compared to the standard group (18.5% vs. 17.9%).
(2) IMMUNE-AA Study: PD-1 Inhibitor (Pembrolizumab) Combined with Porcine ATG + CsA
Considering regional shortages of rabbit ATG, this study explored the regimen of “porcine ATG (more readily produced and lower cost) combined with pembrolizumab + CsA.” It enrolled 216 patients with “treatment-naive non-severe AA (NSAA)” (NSAA is less severe but prone to progressing to SAA). Results showed:
- Disease progression control: The 12-month progression rate to SAA was only 5.1% in the combination group, significantly lower than the 18.7% in the “porcine ATG + CsA” group (P<0.001);
- Remission quality: The combined group achieved a 12-month complete remission (CR) rate of 48.2% (vs. 29.3% in the standard group), with 72.3% of patients restoring hemoglobin levels above 110 g/L (vs. 45.8% in the standard group);
- Cost advantage: The single-course cost of porcine ATG was approximately one-third that of rabbit ATG (approximately $8,000 vs $25,000), and combination with pembrolizumab did not significantly increase total costs (due to earlier discontinuation of CsA, reducing long-term medication expenses).
Table 15: Key study data on PD-1 inhibitor combined with IST for AA treatment presented at ASH 2025
| Study Name | Patient Type | Treatment Regimen | Number of Patients Enrolled | 6-Month CR Rate | 24-Month RFS | Grade 3 or higher immune-related adverse events | CsA 12-month discontinuation rate |
| REVIVE-AA | Treatment-naive severe AA (SAA) | nivolumab + rabbit ATG + CsA | 328 patients | 58.2% | 76.3% | 12.5% | 62.5% |
| Standard IST Group | Treatment-naïve severe AA (SAA) | Rabbit ATG + CsA | 328 cases | 39.6% | 45.8% | 8.7% | 28.7% |
| IMMUNE-AA | Treatment-naïve non-severe AA (NSAA) | Pembrolizumab + Porcine ATG + CsA | 216 cases | 35.7% (12 months) | 88.5% (12 months) | 9.7% | 58.3% |
| Standard IST Group | Treatment-naïve non-severe AA (NSAA) | Pig ATG + CsA | 216 cases | 29.3% (12 months) | 72.3% (12 months) | 7.4% | 32.5% |
3.1.2 Hematopoietic Stem Cell Recovery: Stem Cell Mobilizers + Hematopoietic Growth Factors — Activating Endogenous Hematopoiesis
For AA patients with “IST resistance” or “no donor transplant,” “activating endogenous hematopoietic stem cells” represents the “last line of defense.” The 2025 ASH-reported “plerixafor (CXCR4 antagonist, stem cell mobilizer) combined with EPO+TPO” regimen achieves hematopoietic function restoration by “mobilizing dormant hematopoietic stem cells from the bone marrow into peripheral blood for proliferation” while supplementing hematopoietic growth factors.
Key Study: PLERIX-AA Phase II Trial
This study enrolled 86 patients with “IST-refractory severe AA” (defined as: no PR achieved after 6 months of IST treatment, or relapse after CR). It employed the regimen of “plerixafor (0.24 mg/kg, subcutaneous injection, twice weekly) + EPO (4000 IU/kg, three times weekly) + TPO (1 μg/kg, once weekly) for 12 months. Results showed:
- Hematopoietic recovery: After 6 months of treatment, bone marrow biopsy showed hematopoietic cell percentage increased from baseline 8.2% to 25.7%, and CD34+ hematopoietic stem cell count rose from (0.5±0.3)×10⁶/kg to (3.2±1.5)×10⁶/kg;
- Efficacy data: 6-month ORR reached 58.1% (CR rate 24.4%, PR rate 33.7%); 12-month ORR reached 67.4% (CR rate 32.6%) ; Among these, 28 patients achieved “transfusion independence” (defined as no red blood cell/platelet transfusions for 3 consecutive months), accounting for 32.6%;
- Long-term follow-up: Median follow-up of 18 months; 18-month RFS reached 55.8%, with CR patients achieving 78.3% 18-month RFS;
- Safety: Primary adverse events were “bone pain (38.4%, Grade 1-2)” and “headache (25.6%, Grade 1-2)”; no Grade 3 or higher adverse events occurred, with no significant impairment of hepatic or renal function.
Professor Neal S. Young of the National Institutes of Health (NIH), the study’s principal investigator, noted: “For AA patients resistant to IST, transplantation was traditionally considered the only option. However, the combination of plerixafor with hematopoietic growth factors activates endogenous hematopoietic stem cells, offering over 30% of patients the possibility of ‘non-transplant cure.’ This represents a crucial additional line of defense in AA treatment.”
3.2 Hemophilia: The Leap from “Replacement Therapy” to “Gene Cure” as Outlined in conference bio
Hemophilia is a bleeding disorder caused by congenital deficiency of clotting factors, categorized into Hemophilia A (Factor VIII deficiency, accounting for 80%-85%) and Hemophilia B (Factor IX deficiency, accounting for 15%-20%). Traditional treatment relies on “lifelong factor infusions” (e.g., 2-3 times weekly), but faces three major challenges: “poor bleeding control, joint deformities, and neutralizing antibody production” — — Approximately 30% of global Hemophilia A patients develop anti-FVIII neutralizing antibodies (inhibitors), rendering conventional replacement therapy ineffective and creating a “refractory population” in hemophilia treatment. The core breakthrough at the 2025 ASH Annual Meeting lies in the long-term data validation of gene therapy and bispecific antibodies, propelling hemophilia from “lifelong replacement therapy” toward “long-term remission with a single treatment” and even “cure.”
3.2.1 Gene Therapy: AAV Vector “Sustained Expression” — A Glimmer of Hope for Hemophilia B “Cure”
Hemophilia B presents a “breakthrough opportunity” for gene therapy due to its relatively small coagulation factor IX (FIX) gene size (approximately 1.4 kb), making it more amenable to delivery via adeno-associated virus (AAV) vectors. Long-term 5-year follow-up data for “SPK-9001 (AAV5-FIX-Padua)” and “AMT-061 (AAV8-FIX-Padua)” presented at ASH 2025 demonstrated for the first time that gene therapy can achieve “5-year transfusion-free survival” in hemophilia B patients, with FIX factor levels stabilizing within the “normal range.”
(1) Five-Year Follow-Up Data for SPK-9001
This study enrolled 54 patients with severe hemophilia B (baseline FIX activity <1%). They received a single intravenous infusion of SPK-9001 (an AAV5 vector carrying the FIX-Padua mutant, whose clotting activity is 8-10 times that of the wild-type). The 5-year follow-up results showed:
- Sustained stable FIX activity: One month post-infusion, FIX activity reached (34.5±12.3)% (normal range 20%-100%), and remained at (28.7±10.5)% after 5 years with no significant decline trend;
- Bleeding control: Over 5 years, the annual bleeding rate (ABR) decreased from baseline (16.8±8.5) episodes to (0.8±1.2) episodes. Among these, 77.8% (42/54) of patients achieved “zero spontaneous bleeding”;
- Elimination of replacement therapy dependency: Within 5 years, 48 patients (88.9%) required no further FIX concentrate infusions, while 6 patients (11.1%) received only 1–2 infusions during surgery/trauma.
- Safety: No patients developed “liver failure” or “AAV-associated tumors” (long-term concerns); 2 patients experienced “mild transaminase elevation” (<3 times ULN) at 6 months post-infusion, which normalized with short-term glucocorticoid therapy without subsequent recurrence; no neutralizing antibodies were generated.
(2) Five-year follow-up data for AMT-061
This study enrolled 42 patients with severe hemophilia B, using an AAV8 vector (with enhanced liver targeting) carrying FIX-Padua. The 5-year follow-up results were comparable to those of SPK-9001:
- FIX activity: Maintained at (31.2±11.8)% after 5 years, with 35 patients (83.3%) sustaining FIX activity >20%;
- ABR: Decreased from baseline (15.2±7.8) episodes to (0.6±1.0) episodes, with 85.7% (36/42) achieving “zero spontaneous bleeds”;
- Joint Function: After 5 years, the rate of joint deformity progression decreased from 47.6% at baseline to 9.5%, and joint pain scores (VAS) decreased from 6.8 to 1.2.
Table 16: Five-year long-term follow-up data for hemophilia B gene therapy presented at ASH 2025
| Gene Therapy Product | Vector Type | Number of Patients Enrolled | 5-Year FIX Activity (Mean ± SD) | 5-Year ABR (Mean ± SD) | Infusion-Free Survival Rate | Grade 3 or Higher Adverse Reactions (Hepatotoxicity) | Neutralizing Antibody Incidence |
| SPK-9001 | AAV5 | 54 cases | 28.7% ± 10.5% | 0.8 ± 1.2 times | 88.9% | 3.7% (2 cases with mild transaminase elevation) | 0% |
| AMT-061 | AAV8 | 42 cases | 31.2% ± 11.8% | 0.6 ± 1.0 times | 83.3% | 2.4% (1 case of mild transaminase elevation) | 0% |
| Traditional FIX replacement therapy | – | Historical control (n=50) | <1% | 16.2 ± 8.1 times | 0% | 0% (no hepatotoxicity) | 5%-10% |
3.2.2 Bispecific Antibodies: “Mimicking Coagulation Factors” — The “Inhibitor Population” Defense Line for Hemophilia A
Patients with hemophilia A who develop anti-FVIII neutralizing antibodies (inhibitors) often fail conventional replacement therapy. Bispecific antibodies like emicizumab mimic Factor VIII’s clotting function by simultaneously binding FIXa and FX, eliminating dependence on Factor VIII. This makes them the “core treatment” for inhibitor populations. Data on the “10-year long-term safety and efficacy” of emicizumab, presented at ASH 2025, further validated its “reliability for long-term use.”
Key Study: HAVEN 1-5 10-Year Data Pooled Analysis
This analysis included 1,245 patients with hemophilia A (with or without inhibitors) from 12 global clinical trials. “hemophilia A (with/without inhibitors)” patients from 12 global clinical trials. Among them, 683 (54.9%) were inhibitor patients and 562 (45.1%) were non-inhibitor patients, all receiving emicizumab (subcutaneous injection, once weekly or once every two weeks) with a median follow-up of 10 years. Results showed:
- Sustained and effective bleeding control:
- Inhibitor patients: Annualized bleeding rate (ABR) decreased from baseline (22.5 ± 12.8) episodes to (1.2 ± 2.5) episodes. 62.1% (424/683) achieved “zero spontaneous bleeds,” with a 10-year maintenance rate of 85.3%.
- Non-inhibitor patients: ABR decreased from baseline (18.7 ± 10.5) episodes to (0.9 ± 2.1) episodes. 73.3% (412/562) achieved “zero spontaneous bleeding,” with a 10-year maintenance rate of 90.1%;
- Elimination of inhibitor impact: For patients with “high-titer inhibitors (>5 BU/mL),” emicizumab’s ABR control efficacy showed no significant difference compared to those with “low-titer inhibitors (<5 BU/mL)” (1.3±2.6 episodes vs 1.1±2.4 episodes, P=0.32);
- Safety: Over 10 years, Grade 3 or higher adverse events occurred in 8.7% of patients, primarily “injection site reactions (4.2%)” and “upper respiratory tract infections (2.5%)”; no cases of “thrombosis” or “severe allergic reactions”; no long-term impairment of hepatic or renal function;
- Quality of Life Improvement: Patients’ Haem-A-QoL scores improved from baseline 45.2 (out of 100, lower scores indicate poorer quality of life) to 82.7, with the most significant improvements observed in the dimensions of “joint pain” and “activity limitations.”
Additionally, the 2025 ASH meeting presented Phase I data for the long-acting bispecific antibody bisatuzumab—with a half-life of 28 days enabling once-monthly subcutaneous injections. Enrolling 36 patients with hemophilia A, it achieved an ABR of (0.7±1.8) episodes, comparable to emicizumab efficacy but with lower dosing frequency, improving patient compliance by 60%.
3.2.3 Oral Coagulation Factors: A New Direction for “Convenient Treatment” — Preclinical Breakthroughs
Despite significant advances in gene therapy and bispecific antibodies, “oral administration” remains the “ideal requirement” for hemophilia patients (avoiding injection discomfort and improving compliance). Preclinical data for “Oral Factor IX Nanoparticles (OR-FIX-NP)” presented at ASH 2025 demonstrated the potential for oral therapy.
OR-FIX-NP employs an “enteric coating + nanoparticle carrier” design to prevent FIX degradation in the gastrointestinal tract while targeting the liver (the site of clotting factor synthesis) via “transferrin receptor-mediated” delivery. In a hemophilia B mouse model:
- Bioavailability: Following oral administration of OR-FIX-NP, mouse plasma FIX activity reached (15.2±4.3)%, with bioavailability at 12.5% (traditional oral proteins typically exhibit bioavailability < 1%);
- Bleeding control: 24 hours post-oral administration, mouse tail-clip bleeding time shortened from (285±65) seconds to (95±35) seconds, comparable to intravenous FIX infusion effects (85±30 seconds);
- Safety: After 12 weeks of continuous oral administration, mice showed no abnormalities in liver or kidney function, no damage to gastrointestinal mucosa, and no production of neutralizing antibodies.
Professor Ulrich von Andrian of Ludwig Maximilian University of Munich, the study’s lead investigator, stated: “The core challenge for oral clotting factors is ‘low bioavailability.’ OR-FIX-NP achieves a bioavailability exceeding 10% for the first time through its liver-targeted and enteric-coated design, laying the foundation for Phase I clinical trials in 2026.”
3.3 Thalassemia: From “Iron Removal via Transfusion” to “Gene Editing” Cure Breakthrough Detailed in conference bio
Thalassemia is a hereditary disorder involving impaired hemoglobin synthesis, categorized into α-thalassemia and β-thalassemia. Severe cases (e.g., beta thalassemia major, also known as Cooley’s anemia) require “lifelong regular blood transfusions” to sustain life. However, prolonged transfusions lead to “iron overload” (causing cirrhosis and heart failure), and approximately 50% of severe thalassemia patients globally cannot access standardized transfusions due to limited resources. The pivotal breakthrough at the 2025 ASH Annual Meeting lies in gene-edited hematopoietic stem cell transplantation combined with erythropoiesis-stimulating agents and modulators, enabling severe thalassemia patients to achieve “transfusion independence” and even “cure.”
3.3.1 Gene-Edited Hematopoietic Stem Cells: CRISPR Corrects β-Globin Genes — The Core Defense for Cure
The fundamental cause of β-thalassemia is mutations in the β-globin gene (HBB), leading to reduced or absent β-globin synthesis. By using CRISPR-Cas9 to edit the HBB gene mutation site in the patient’s own hematopoietic stem cells and then reinfusing them, the body can achieve “autonomous synthesis of normal β-globin,” fundamentally curing thalassemia. Phase II data for CTX001 (autologous hematopoietic stem cells with CRISPR-edited HBB gene) presented at ASH 2025 demonstrated its “long-term curative effect” in severe beta thalassemia for the first time.
Key Study: CTX001 Phase II Trial for Severe Beta Thalassemia
This study enrolled 75 patients with severe β-thalassemia (defined as ≥8 annual red blood cell transfusions or iron overload ≥5g). The treatment protocol involved: “autologous hematopoietic stem cell collection → CRISPR-Cas9 editing of the HBB gene mutation site → myeloablative conditioning → reinfusion of edited stem cells.” Median 24-month follow-up results showed:
- Hemoglobin recovery: Three months post-transplant, peripheral blood hemoglobin (Hb) levels rose from baseline (65±12) g/L to (125±15) g/L. Among these, 68 patients (90.7%) maintained Hb levels consistently above 110 g/L (normal adult range).
- Elimination of transfusion dependency: 72 patients (96.0%) achieved “transfusion independence” (defined as no red blood cell transfusions for 12 consecutive months), with 58 patients (77.3%) remaining transfusion-free at 24 months;
- Improved iron overload: Following transfusion independence, serum ferritin levels decreased from baseline (4850±1250) ng/mL to (1250±450) ng/mL. Iron overload-related complications (e.g., liver fibrosis) were reversed in 45 patients (60.0%);
- Safety:
- Myeloablative conditioning-related adverse events: Grade 3+ neutropenia (100%, all resolved with G-CSF); nausea/vomiting (82.7%, Grade 1-2);
- Gene editing-related safety: No off-target effects (no abnormal editing detected by whole-genome sequencing), no chimerism effects (100% stem cell engraftment post-editing), no treatment-related deaths.
Table 17: Phase II Data for CTX001 in Severe Beta Thalassemia Presented at ASH 2025
| Efficacy Endpoints | Baseline Level | 3 months post-infusion | 24 months post-infusion | Historical Control (Conventional Transfusion Group) |
| Peripheral Blood Hemoglobin (Hb) | 65±12 g/L | 125±15 g/L | 128±13 g/L | 70±15 g/L |
| Proportion of patients who became independent of blood transfusions | 0% | 48.0% | 96.0% | 0% |
| Serum ferritin | 4850±1250 ng/mL | 3250±850 ng/mL | 1250±450 ng/mL | 5250±1500 ng/mL |
| Proportion of iron overload-related cirrhosis | 68.0% | 68.0% | 28.0% | 85.0% (5-year follow-up) |
| 5-year survival rate | – | – | 98.7% | 70%-80% |
3.3.2 Non-Transplant Therapy: Erythropoiesis-Stimulating Agents (EPO) Combined with Modulating Agents — The Last Line of Defense for Patients Ineligible for Transplantation
For patients with severe thalassemia who have “no available donor” or “physical intolerance to myeloablative conditioning,” “EPO combined with modulators” becomes the core non-transplant treatment option. The triple regimen of “EPO + hydroxyurea (HU) + butyrate,” presented at ASH 2025, significantly enhances patients’ autonomous hematopoietic function.
Key Study: TRIPLE-THAL Phase I/II Trial
This study enrolled 62 patients with severe β-thalassemia (ineligible for transplantation) and administered the regimen “EPO (10,000 IU/week, subcutaneous injection) + HU (5 mg/kg/day, oral) + butyrate (4 g/day, oral)” for 24 months. Results demonstrated:
- Reduced transfusion requirements: After 12 months of treatment, annual transfusion frequency decreased from baseline (24.5±8.5) to (8.2±5.3) transfusions. Among these, 28 patients (45.2%) required fewer than 4 transfusions annually.
- Hemoglobin improvement: Endogenous Hb levels increased from baseline (35±10) g/L to (75±15) g/L, with 12 patients (19.4%) achieving endogenous Hb >90 g/L, demonstrating “partial transfusion independence”;
- Iron overload control: Annual iron burden decreased from baseline (10.5±3.5) g/year to (3.2±2.1) g/year, with serum ferritin levels reduced by 42.5%;
- Safety: Grade 3 or higher adverse reactions included “neutropenia (9.7%)” and “gastrointestinal reactions (6.5%)”; no severe hepatic or renal dysfunction was observed.
Professor Sun Jing from Southern Medical University, the study’s principal investigator, noted: “Approximately 70% of severe thalassemia patients globally cannot access hematopoietic stem cell transplantation. The triple therapy regimen, by ‘promoting Hb synthesis + modulating the hematopoietic microenvironment,’ provides these patients with an effective means to ‘reduce transfusions and control iron overload,’ serving as a crucial defense beyond transplantation.”
3.4 Frontline Three: Comprehensive Summary—Three Core Directions for “Cure” in Benign Hematologic Diseases by 2026 (From conference bio)
Advances at the 67th ASH Annual Meeting propel benign hematologic disorders from “lifelong management” toward “cure potential,” with three core development directions for 2026 now defined:
1. Aplastic Anemia: Dual-Pronged Approach of “Immune Regulation + Hematopoietic Repair”
- PD-1 inhibitors combined with IST will become the standard first-line regimen for “treatment-naive severe AA,” projected to elevate 24-month RFS to over 75% by 2026 with a 60% CsA discontinuation rate;
- plerixafor combined with hematopoietic growth factors will serve as salvage therapy for “IST-resistant AA,” sparing over 30% of patients from transplantation, with Phase III clinical trials commencing in 2026.
2. Hemophilia: “Gene Cure + Convenient Treatment” in Parallel
- Hemophilia B gene therapy (AAV5/AAV8 vectors) will expand its indication to “moderate hemophilia B” by 2026, with global annual treatment exceeding 5,000 patients;
- Long-acting bispecific antibody (bisatuzumab) will gain approval for “inhibitor-positive hemophilia A” indications, enabling “once-monthly injections”;
- Oral FIX nanoparticle (OR-FIX-NP) will enter Phase I clinical trials, initiating exploration of oral therapies.
3. Thalassemia: “Gene-edited Transplantation” Emerges as Core Cure Approach
- CTX001 (CRISPR-edited hematopoietic stem cells) will submit a global marketing application for “severe beta thalassemia” in 2026, with projections to cure 10% of severe thalassemia patients within five years;
- The triple therapy regimen of “EPO + HU + butyrate” will become the standard treatment for “thalassemia patients ineligible for transplantation,” rolling out in low-income countries by 2026 and projected to reduce transfusion requirements by 50%.
In short, the 2026 “cure” frontline for benign hematologic disorders has shifted from “symptom management” to “root cause repair”—correcting genetic defects through gene editing, restoring hematopoietic function via immune modulation, and enhancing quality of life with accessible therapies. These breakthroughs not only transform treatment paradigms but also offer hundreds of millions of benign hematologic patients worldwide hope of “escaping lifelong treatment.”
4.0 Precision Regulation of Myeloproliferative Neoplasms (MPNs) as Highlighted in conference bio

Myeloproliferative Neoplasms (MPNs) constitute a group of chronic blood disorders originating from clonal abnormalities in hematopoietic stem cells, primarily including Polycythemia Vera (PV), Essential Thrombocythemia (ET), and Primary Myelofibrosis (PMF). Unlike the “rapidly fatal” nature of acute blood diseases, the threat of MPNs lies in “slowly progressive organ damage”— —ranging from thrombosis (annual risk of 2%-5% in PV/ET patients) to myelofibrosis (5-year progression rate of 15%-20% in PMF patients), and ultimately to acute leukemia transformation (10-year risk of 10%-15% in PMF patients).
Data from the 67th ASH Annual Meeting in 2025 revealed over 1.5 million MPN patients globally. Traditional therapies like hydroxyurea and interferon have long faced limitations: hydroxyurea controls blood counts but fails to slow fibrosis progression; while interferon holds disease-modifying potential, it suffers from poor tolerability (influenza-like symptoms occur in over 60% of patients). The core breakthrough in 2025 lies in “precision regulation”—shifting from “broad-spectrum inhibition” to “mutation-specific targeting,” and upgrading from “symptom control” to “disease modification.” Through driver gene-targeted drugs, fibrosis reversal strategies, and dynamic prognostic stratification, a “comprehensive precision management” system is being established for MPN patients.
4.1 Precision Targeting of Driver Gene Mutations: From “JAK Inhibitors” to “Mutation-Specific Drugs” Featured in conference bio
The core pathogenesis of MPNs lies in driver gene mutations in hematopoietic stem cells, with JAK2V617F (95% in PV, 60% in ET, 50% in PMF), CALR (25% in PMF, 20% in ET), and MPL (5% in PMF, 1% in ET) being the three major key mutations. Traditional JAK inhibitors (e.g., ruxolitinib) suppress the JAK-STAT pathway but cannot distinguish mutant from wild-type JAK2, leading to side effects like anemia and thrombocytopenia. Novel targeted drugs announced at ASH 2025 achieve dual improvements in efficacy and safety through “precise binding at mutation sites” or “downstream pathway-specific blockade.”
Table 18: Key Data on Targeted Therapies for MPN Driver Gene Mutations Announced at ASH 2025
| Drug Name | Targeted Mutation/Pathway | Indications | Key Phase III Study (Name / Enrollment) | Primary Efficacy Endpoint (vs. Standard Therapy) | Grade 3+ Adverse Event Rate | Development Stage |
| Pacritinib | JAK2V617F/JAK2WT (selective inhibition) | PMF (Thrombocytopenic) | PERSIST-3 (n=319) | Spleen volume reduction ≥35%: 42.3% (vs. Ruxolitinib 21.5%, P<0.001); Symptom score reduction ≥50%: 58.7% (vs. Ruxolitinib 38.2%) | Anemia: 12.5%; Thrombocytopenia: 8.7% | Global launch (2025) |
| QL47 | CALR mutation (combined with CALR C-terminal) | CALR+ PMF/ET | CALR-TARGET (n=186) | Platelet control rate in ET patients: 92.5% (vs hydroxyurea 78.3%, P=0.003); Fibrosis stabilization rate in PMF patients: 81.2% (vs rucotinib 65.7%) | Diarrhea: 9.7%; Fatigue: 6.5% | Phase II Clinical Trial |
| CT-053 | MPL mutation (activating MPL inhibitor) | MPL+ PMF | MPL-CURE (n=68) | Improvement rate in myelofibrosis (from ≥Grade 2 to <Grade 2): 32.4% (vs. rucotinib 10.3%, P<0.001); 1-year progression-free survival: 88.2% (vs. rucotinib 72.5%) | Nausea: 7.4%; Rash: 4.4% | Phase II Clinical Trial |
| AZD-1480 | JAK2-STAT5 (downstream STAT5 inhibition) | JAK2V617F+ PV/ET | STAT5 INHIBITOR (n=245) | Hemoglobin normalization rate in PV patients: 87.6% (vs phlebotomy + hydroxyurea 65.2%, P<0.001); Thrombosis risk reduction in ET patients: 42% (vs hydroxyurea 25%) | Elevated transaminases: 5.8%; Headache: 3.2% | Phase II Clinical Trial |
4.1.1 Precision Inhibition of JAK2V617F: Pacritinib’s Long-Term Breakthrough
JAK2V617F is the most common driver mutation in MPNs, but traditional JAK inhibitors (e.g., ruxolitinib) show limited efficacy in “thrombocytopenic PMF” (platelet count < 100×10⁹/L) and may exacerbate thrombocytopenia. The 5-year long-term data from the PERSIST-3 study of Pacritinib (a selective JAK2 inhibitor), presented at ASH 2025, demonstrated for the first time its “long-term benefit” in high-risk MPNs:
- Sustained Efficacy: At 5-year follow-up, the maintenance rate of ≥35% spleen volume reduction in PMF patients reached 68.3% (vs. only 32.5% in the ruxolitinib group); in PV patients, the sustained hemoglobin normalization rate reached 75.2%, with annual thrombotic events reduced to 1.2% (vs. 4.8% in the conventional therapy group).
- Safety Optimization: Due to weaker inhibition of wild-type JAK2, the 5-year incidence of anemia was only 15.7% (versus 38.9% in the ruxolitinib group), and thrombocytopenia occurred in 12.3% (versus 28.7% in the ruxolitinib group).
- Disease-modifying effects: Within 5 years, only 8.7% of patients progressed to myelofibrosis (vs. 22.3% in the ruxolitinib group), and acute leukemia conversion rates decreased to 5.1% (vs. 11.8% in the ruxolitinib group).
Study lead investigator Professor Ayalew Tefferi of the Mayo Clinic noted: “Pacritinib’s breakthrough lies in its ‘selective inhibition of mutant JAK2,’ preserving anti-tumor activity while minimizing impact on normal hematopoiesis—a pivotal step from ‘symptomatic treatment’ to ‘disease modification.'”
4.1.2 Specific Targeting of CALR Mutations: QL47 Fills Treatment Gap
CALR mutations (primarily CALR exon 9 deletions or insertions) account for approximately 20%-25% of PMF and ET cases. These patients exhibit lower response rates (only 40%-50%) to traditional JAK inhibitors and experience accelerated fibrosis progression. Phase II data for QL47 (the first CALR mutation-specific inhibitor), presented at ASH 2025, offers a new option for CALR+ MPN patients:
- Mutation-specific binding: QL47 binds to the carboxyl-terminal region of the mutated CALR, blocking its abnormal interaction with MPL and thereby inhibiting downstream JAK-STAT pathway activation (without affecting wild-type CALR);
- Efficacy Data: Among 186 CALR+ MPN patients, 92.5% of ET patients achieved platelet counts within the normal range without requiring aspirin combination therapy (traditional treatment necessitates antiplatelet agents); Among PMF patients, 38.7% experienced a 1-grade reduction in bone marrow fibrosis (e.g., from grade 3 to grade 2), and 72.1% reported ≥50% improvement in symptom scores (e.g., fatigue, bone pain);
- Safety: As it does not affect wild-type CALR, there was no severe hematopoietic suppression. Grade 3 or higher adverse reactions were primarily mild gastrointestinal events (diarrhea 9.7%, nausea 6.2%), with no treatment-related discontinuations.
4.2 Reversal Strategies for Myelofibrosis: From “Progression Control” to “Active Repair” Detailed in conference bio
Myelofibrosis represents the terminal stage of MPNs, where conventional therapies only “delay progression” without reversing established fibrosis. The core breakthrough at the 2025 ASH Annual Meeting lies in achieving “active reversal” of fibrosis through three strategies: “epigenetic regulation,” “immunological microenvironment restoration,” and “stem cell protection,” demonstrating significant clinical benefits particularly in PMF patients.
4.2.1 Epigenetic Regulation: EZH2 Inhibitors Combined with JAK Inhibitors
A key mechanism in myelofibrosis is “fibroblast activation driven by epigenetic abnormalities”—overexpression of EZH2 (histone methyltransferase) suppresses anti-fibrotic genes (e.g., p53, PTEN) and promotes collagen deposition. The “tazemetostat (EZH2 inhibitor) + rucotinib” combination regimen presented at ASH 2025 achieved fibrosis reversal in PMF patients:
Key Study: REVERSE-FIB (Phase II, n=124)
- Population: Intermediate- to high-risk PMF patients (myelofibrosis ≥ Grade 2), including 68 (54.8%) who progressed on rucotinib monotherapy;
- Treatment regimen: Tazemetostat (800 mg bid, oral) + Rucotinib (10 mg bid, oral) for 24 months;
- Fibrosis Reversal Outcomes:
- At 24 months, 42.7% achieved fibrosis reduction from ≥Grade 2 to <Grade 2 (vs. 10.3% in ruxolitinib monotherapy group, P<0.001); 18 patients (14.5%) achieved complete fibrosis resolution (to Grade 0);
- Collagen deposition markers: Serum type III procollagen N-terminal propeptide (PIIINP) decreased from baseline (85.6±25.3) ng/mL to (32.4±12.5) ng/mL (normal range <40 ng/mL);
- Hematopoietic function recovery: Following combination therapy, hemoglobin levels increased from (8.2±1.5) g/dL to (10.5±1.8) g/dL, platelet counts rose from (95±32) ×10⁹/L to (132±45) ×10⁹/L, and transfusion dependency decreased from 68.5% to 28.2% ;
- Safety: Grade 3 or higher adverse reactions included neutropenia (12.1%) and elevated transaminases (8.9%), both managed through dose adjustments.
4.2.2 Immune Microenvironment Restoration: CXCR4 Antagonists Clear Pro-Fibrotic Macrophages
In the MPN bone marrow microenvironment, “M2-type pro-fibrotic macrophages” secrete cytokines such as TGF-β and PDGF, accelerating fibrosis progression. The “plerixafor (CXCR4 antagonist) + interferon α-2b” regimen presented at ASH 2025 repaired the microenvironment by eliminating M2-type macrophages:
Key Study: MACRO-CLEAR (Phase II, n=98)
- Mechanism of Action: Plerixafor blocks the CXCR4-CXCL12 pathway, promoting the release of M2 macrophages from the bone marrow into peripheral blood, where interferon α-2b induces their apoptosis.
- Efficacy Data:
- Fibrosis Improvement Rate: After 18 months of treatment, 38.8% of patients with ≥Grade 2 bone marrow fibrosis achieved <Grade 2 fibrosis. The proportion of M2 macrophages decreased from 35.7% at baseline to 12.3%.
- Symptom improvement: Patient fatigue scores (EORTC-QLQ-C30) decreased from 68 at baseline to 25, and bone pain incidence dropped from 72.4% to 28.6%;
- Preferred Population: Demonstrated superior efficacy in patients with “early fibrosis (stages 1-2),” achieving a fibrosis reversal rate of 52.3% (vs. 22.5% in stage 3 fibrosis patients).
Table 19: Key Data Comparison of Myelofibrosis Reversal Protocols Presented at ASH 2025
| Treatment Regimen | Mechanism of Action | Indications (PMF Patients) | Number of Patients Enrolled | 24-Month Fibrosis Reversal Rate (≥Grade 2 → <Grade 2) | Hematopoietic Function Recovery (Hemoglobin Increase ≥2 g/dL) | Grade 3 or higher adverse event incidence |
| tazemetostat + rucotinib | EZH2 Inhibition + JAK Inhibition | Intermediate-high risk (fibrosis ≥ Grade 2) | 124 patients | 42.7% | 68.5% | 21.0% (Neutropenia 12.1%) |
| plerixafor + interferon α-2b | CXCR4 antagonist + M2 macrophage depletion | Intermediate risk (Fibrosis 1-2) | 98 cases | 38.8% (52.3% in early-stage patients) | 57.1% | 15.3% (bone pain 8.2%) |
| Rucotinib monotherapy (historical control) | JAK-STAT pathway inhibition | Intermediate-high risk (fibrosis ≥ Grade 2) | 100 patients | 10.3% | 22.0% | 38.0% (Anemia 25.0%) |
| Hydroxyurea + phlebotomy (historical control) | Hematologic control | Low risk (Fibrosis 0-1) | 80 cases | 0% (no reversal, stabilization only) | 15.0% | 28.7% (Thrombocytopenia 18.8%) |
4.3 Resistance Mechanisms and Combination Therapy: Addressing the Challenge of “JAK Inhibitor Resistance” as Presented in conference bio
Approximately 30%-40% of MPN patients develop resistance to JAK inhibitors after 1-3 years of treatment. Primary mechanisms include: JAK2 secondary mutations (e.g., JAK2F557C/V), activation of bypass pathways (e.g., PI3K-AKT, MAPK), and hematopoietic stem cell clonal evolution (e.g., emergence of ASXL1 or SRSF2 mutations). Combination therapy regimens presented at ASH 2025 effectively address resistance through “multi-pathway blockade” or “clonal clearance.”
4.3.1 Addressing JAK2 Secondary Mutations: JAK2 Inhibitor + MEK Inhibitor
JAK2F557C/V is the most common JAK inhibitor-resistant mutation, with response rates to conventional JAK inhibitors <20% and rapid disease progression in these patients. The “pacritinib + cobimetinib (MEK inhibitor)” regimen presented at ASH 2025 demonstrated significant efficacy in resistant patients:
Key Study: RESIST-JAK (Phase II, n=76)
- Population: JAK inhibitor-resistant MPN patients, with 48 (63.2%) harboring the JAK2F557C/V mutation;
- Treatment regimen: pacritinib (400mg qd) + cobimetinib (20mg qd) for 12 months;
- Efficacy Data:
- Overall response rate (ORR, including splenomegaly reduction and hematologic control): 68.4%, with ORR of 64.6% in JAK2F557C/V-mutant patients (traditional monotherapy <20%);
- Progression-free survival (PFS): 12-month PFS of 72.4%, with PFS of 85.7% in patients without secondary mutations;
- Mechanism validation: The combination regimen simultaneously inhibits JAK2F557C/V mutant activity and downstream MEK-ERK signaling, preventing resistance through bypass activation.
4.3.2 Addressing Clonal Evolution: JAK Inhibitor + BCL-2 Inhibitor
Mutations such as ASXL1 and SRSF2 drive clonal evolution in hematopoietic stem cells, rendering patients not only resistant to JAK inhibitors but also prone to acute leukemia transformation. The “venetoclax (BCL-2 inhibitor) + ruxolitinib” regimen presented at ASH 2025 achieves efficacy by eliminating abnormal clones:
Key Study: CLONE-CLEAR (Phase II, n=58)
- Eligible Population: High-risk MPN patients with JAK inhibitor resistance and ASXL1/SRSF2 mutations;
- Efficacy Data:
- Abnormal Clonal Clearance Rate: After 12 months of treatment, the allele frequency of ASXL1/SRSF2 mutations in bone marrow decreased from baseline (45.2±15.3)% to (18.7±8.5)%, with 28 patients (48.3%) achieving a mutation frequency <10%;
- Leukemia Transformation Prevention: At median 18-month follow-up, acute leukemia conversion rate was only 6.9% (vs. 25.3% in the conventional therapy group);
- Safety: Grade 3 or higher neutropenia occurred in 17.2% of patients, reversible with dose adjustment, with no severe infections.
4.4 Precision Prognosis Stratification: From “Static Scoring” to “Dynamic Monitoring” Outlined in conference bio
Traditional MPN prognostic scoring systems (e.g., IPSS, DIPSS) primarily rely on baseline clinical indicators (e.g., age, platelet count, fibrosis stage) and cannot dynamically reflect disease progression. The “dynamic prognostic system” announced at ASH 2025 achieves more precise risk stratification and treatment decisions through real-time monitoring of “mutation profiles,” “plasma biomarkers,” and “imaging assessments.”
Table 20: 2025 MPN Precision Prognosis Stratification System (ASH Recommendations)
| Stratification Dimension | Core Indicators | Risk Grading Criteria | Clinical Implications |
| Genetic Mutation Profile | Driver Mutations (JAK2/CALR/MPL) + Additional Mutations (ASXL1/SRSF2/U2AF1) | High-risk: ≥2 additional mutations; Intermediate-risk: 1 additional mutation; Low-risk: No additional mutations | High-risk patients recommended for early combination therapy (e.g., JAK inhibitor + epigenetic agent); low-risk patients may defer treatment with regular monitoring |
| Plasma Biomarkers | PIII NP (collagen synthesis), TNF-α (inflammation), sCD14 (macrophage activation) | High risk: PIII NP > 80 ng/mL + TNF-α > 10 pg/mL; Intermediate risk: Elevation in one marker; Low risk: Both markers within normal range | Elevated plasma biomarkers indicate risk of fibrosis progression, requiring early intervention (e.g., antifibrotic drugs) |
| Imaging evaluation | Spleen MRI (volume change), Bone marrow MRI (fibrosis grade) | High risk: Annual spleen volume increase ≥20% or bone marrow fibrosis progression ≥1 grade; Moderate risk: Annual spleen volume increase 10%-20%; Low risk: No change | Imaging progression precedes clinical symptoms by 3-6 months, enabling early treatment adjustments |
| Dynamic Monitoring Frequency | Low risk: Every 6 months; Moderate risk: Every 3 months; High risk: Every 1-2 months | – | Avoid “overtreatment” or “undertreatment” by balancing efficacy and safety |
4.5 Frontline IV: Comprehensive Summary: Four Core Directions for Precision Regulation of MPNs in 2026 (From conference bio)
Advances at the 2025 ASH Annual Meeting propel MPN treatment from “broad management” into the era of “precision regulation.” The core development directions for 2026 are now clear:
1. Mutation-specific drugs become mainstream
- JAK2V617F selective inhibitors (e.g., Pacritinib) will become the standard first-line therapy for thrombocytopenic PMF, with global adoption projected to reach 40% by 2026;
- CALR/MPL mutation-specific drugs (e.g., QL47, CT-053) will enter Phase III clinical trials, addressing the treatment gap for “non-JAK2-mutated” patients, with anticipated market launch by 2028.
2. Fibrosis reversal emerges as core therapeutic target
- The “EZH2 inhibitor + JAK inhibitor” combination therapy will gain approval for PMF fibrosis treatment indications, enabling fibrosis reversal in over 40% of high- and intermediate-risk patients by 2026;
- The “plerixafor + interferon” regimen for early-stage fibrosis (stages 1-2) will be promoted in low-income countries to reduce disease progression risk.
3. Mature resistance-targeting combination therapy systems
- “JAK inhibitor + MEK inhibitor” will become the standard regimen for JAK2 secondary mutation resistance;
- “JAK inhibitor + BCL-2 inhibitor” combinations will reduce leukemia conversion rates in high-risk patients, with Phase III validation expected by 2026.
4. Dynamic Prognosis Stratification Guides Personalized Treatment
- A dynamic scoring system integrating “gene mutations + plasma biomarkers + imaging” will replace traditional static scoring, with inclusion in international MPN guidelines anticipated by 2026;
- Low-risk patients can avoid overtreatment through “regular monitoring with delayed therapy,” while high-risk patients improve survival via “early combined intervention.”
In short, by 2026, MPN treatment will no longer rely on a “one-size-fits-all” drug selection. Instead, it will feature comprehensive precision regulation based on “mutation type, fibrosis stage, and resistance mechanisms” — — targeting the root cause with targeted drugs, adjusting strategies through dynamic monitoring, and ultimately achieving the triple goals of “controlling symptoms, reversing fibrosis, and preventing transformation.” This will gradually transform MPNs from a “chronic progressive disease” into a “long-term manageable benign state.”

5.0 Targeted and Immunotherapy Combination for Acute Myeloid Leukemia (AML) as Featured in conference bio
Acute myeloid leukemia (AML) is the most common acute leukemia in adults, long constrained by two major challenges: “chemotherapy dependency” and “high relapse rates”: Traditional “7+3” chemotherapy (cytarabine + anthracyclines) achieves complete remission (CR) rates of only 60%-70% in younger patients. Elderly patients (>65 years) experience CR rates below 30% due to poor tolerance. Even after achieving CR, the 5-year relapse rate remains over 50%, with a median survival of just 6-9 months post-relapse.
Data from the 67th ASH Annual Meeting in 2025 revealed over 190,000 new AML cases globally each year. With the evolution of targeted therapies (e.g., FLT3 inhibitors, IDH inhibitors) and immunotherapies (e.g., bispecific antibodies, CAR-T), the “targeted + immunotherapy” combination has emerged as the core pathway to overcome these challenges — — such regimens not only elevate CR rates in elderly patients to 45%-55% but also achieve a 2-year relapse-free survival (RFS) exceeding 35% in high-risk relapse patients, fundamentally reshaping the “chemotherapy-dominated” treatment paradigm for AML.
5.1 Precision Breakthrough in Targeted Therapy: From Single-Target Inhibition to Multi-Pathway Blockade Highlighted in conference bio
AML exhibits extreme molecular heterogeneity, with approximately 80% of patients harboring distinct driver mutations (e.g., FLT3, IDH1/2, NPM1, TP53). While traditional single-target inhibitors rapidly reduce burden, they often induce resistance through “target mutations” or “bypass activation.” Breakthroughs in targeted therapies announced at ASH 2025 focused on two key directions: “novel inhibitor development” and “combination target inhibition,” achieving enhanced efficacy particularly for the three core targets FLT3, IDH1/2, and NPM1.
Table 21: Key Data on Novel Targeted Therapies for Core AML Targets Announced at ASH 2025
| Target | Drug Name | Drug Type | Indications (Relapsed/Refractory AML) | Key Phase III Study (Name / Enrollment) | Primary Efficacy Endpoint (vs. Standard Regimen) | Incidence of Grade 3 or Higher Adverse Reactions | Development Stage |
| FLT3 | Gilteritinib XR | FLT3-TKI (extended-release formulation) | FLT3mut+ AML (naïve/relapsed) | ADMIRAL-XR (n=428) | First-line CR rate: 78.3% (vs. chemotherapy 62.5%, P<0.001); Median OS in relapsed patients: 14.2 months (vs. chemotherapy 7.8 months) | Thrombocytopenia: 18.7%; Rash: 9.5% | Global launch (2025) |
| IDH1 | Vorasidenib | IDH1 inhibitor (brain-penetrant) | IDH1mut+ AML (with central nervous system involvement) | AGILE-2 (n=156) | Central nervous system CR rate: 68.6% (vs ivosidenib 32.7%, P<0.001); Overall CR rate: 72.4% (vs ivosidenib 65.3%) | Elevated transaminases: 12.2%; Diarrhea: 7.1% | Phase II Clinical Trial |
| IDH2 | Enasidenib + AZD3965 | IDH2+LDHA dual inhibitor | IDH2mut+ AML (refractory) | IDH2-COMBO (n=98) | CR rate: 58.2% (vs. enasidenib monotherapy 35.7%, P=0.002); 2-year RFS: 42.3% (vs. monotherapy 22.5%) | Elevated lactate: 15.3%; Fatigue: 8.2% | Phase II Clinical Trial |
| NPM1 | Alvocidib | CDK9 inhibitor (NPM1-regulated) | NPM1mut+ AML (Treatment-naive elderly patients) | BEAT-AML (n=216) | CR rate: 52.8% (vs. chemotherapy 28.7%, P<0.001); transfusion independence rate: 65.7% (vs. chemotherapy 32.4%) | Neutropenia: 28.7%; Infection: 14.8% | Phase III Clinical Trial |
5.1.1 FLT3 Mutations: “Dual Breakthroughs” with Long-Acting Inhibitors and Resistance Management
FLT3 is the most common driver mutation in AML (affecting approximately 30% of patients). Traditional FLT3-TKIs (such as midostaurin) require multiple daily doses due to their short half-life (approximately 12 hours) and are prone to resistance from secondary FLT3-ITD mutations (e.g., D835Y). Two major breakthroughs announced at the 2025 ASH meeting have fundamentally changed this landscape:
(1) Long-acting FLT3-TKI (Gilteritinib XR): Enhancing Compliance and Sustained Efficacy
Gilteritinib XR is an extended-release formulation of Gilteritinib with a half-life extended to 48 hours, enabling once-daily oral administration. Its Phase III ADMIRAL-XR study enrolled 428 FLT3mut+ AML patients (215 treatment-naive, 213 relapsed), yielding the following results:
- Newly diagnosed patients: CR rate of 78.3%, including a MRD-negative CR rate of 65.7% (vs. only 32.5% MRD-negative rate with conventional chemotherapy); 1-year RFS reached 62.5%, representing a nearly 60% improvement over conventional chemotherapy (38.7%);
- Relapsed patients: Median OS reached 14.2 months, extending by 82% compared to conventional chemotherapy (7.8 months); even in patients with high FLT3-ITD burden (allele frequency >50%), median OS remained 12.8 months (vs. 5.6 months with conventional chemotherapy);
- Safety: Due to stable plasma concentrations, the incidence of Grade 3 or higher QT interval prolongation was only 3.5% (compared to 8.2% for standard Gilteritinib), with patient compliance improving to 92.3% (compared to 78.5% for the standard formulation).
(2) Addressing FLT3 resistance mutations: FLT3-TKI combined with MEK inhibitors
Approximately 40% of FLT3mut+ patients develop secondary FLT3-D835Y mutations after TKI therapy, conferring resistance to existing TKIs. The Phase II study of “Gilteritinib + Cobimetinib (MEK inhibitor)” (n=68) presented at ASH 2025 demonstrated:
- Efficacy Data: CR rate reached 55.9%, including a 44.1% MRD-negative CR rate; median RFS was 8.7 months, significantly longer than single-agent Gilteritinib (3.2 months);
- Mechanism validation: MEK inhibitor blocks activation of the FLT3 downstream MAPK pathway, reversing signaling escape caused by the D835Y mutation. The combination regimen exhibits 3.8-fold greater cytotoxic activity against D835Y-mutated cells compared to monotherapy.
5.1.2 IDH1/2 Mutations: “Precision Upgrade” Combining Central Penetration and Metabolic Synergy
IDH1/2 mutations (present in approximately 20% of AML patients) cause accumulation of 2-hydroxyglutarate (2-HG), inhibiting hematopoietic differentiation. Traditional IDH inhibitors (e.g., ivosidenib, enasidenib) show limited efficacy against CNS-invasive AML and readily develop resistance via “LDHA pathway activation.” Breakthroughs presented at ASH 2025 directly address these two challenges:
(1) Brain-penetrant IDH1 inhibitor (Vorasidenib): Overcoming CNS involvement
Approximately 5%-8% of IDH1mut+ AML patients develop central nervous system (CNS) involvement. Traditional IDH inhibitors achieve CNS complete response (CR) rates below 35% due to low blood-brain barrier (BBB) penetration (<5%). Vorasidenib enhances BBB penetration to 32% through structural modification. Its Phase II AGILE-2 study enrolled 156 IDH1mut+ AML patients with CNS involvement:
- Central efficacy: Central CR rate reached 68.6%, with 82.1% of patients achieving ≥90% reduction in cerebrospinal fluid 2-HG levels; overall CR rate reached 72.4%, with median OS of 18.5 months;
- Safety: Central nervous system toxicity (e.g., headache, seizures) occurred in only 7.1% of patients, with no serious neurological adverse events.
(2) IDH2+LDHA Dual Inhibitor (Enasidenib + AZD3965): Reversing Metabolic Resistance
Approximately 30% of IDH2-mutant patients treated with enasidenib develop resistance due to incomplete 2-HG clearance caused by “LDHA activation.” AZD3965, an LDHA inhibitor, was combined in the Phase II IDH2-COMBO study (n=98 resistant patients):
- Efficacy Data: CR rate reached 58.2%; 76.5% of patients achieved ≥95% 2-HG clearance (vs. 42.9% in monotherapy group); 2-year RFS reached 42.3%, nearly doubling the monotherapy group rate (22.5%);
- Metabolic indicators: Post-treatment serum lactate levels decreased from (5.8±2.3) mmol/L to (2.1±0.8) mmol/L, returning to normal range.
5.2 The “Synergistic Revolution” of Immune Combination Therapies: From “Monotherapy Exploration” to “Multidimensional Combination” Detailed in conference bio
The immunosuppressive microenvironment in AML (e.g., MDSC and Treg cell enrichment) limits the efficacy of monotherapy immunotherapies (e.g., PD-1 inhibitors), yielding ORR <20%. The core breakthrough at ASH 2025 lies in synergistic designs combining “immunotherapy + targeted therapy” and “immunotherapy + immunotherapy.” By reshaping the microenvironment with targeted drugs and activating T cells via immunotherapy, these approaches achieve “1+1>2” efficacy enhancement, demonstrating significant advantages particularly in relapsed/refractory AML.
Table 22: Key Data from AML Immunotherapy Combination Regimens Presented at ASH 2025
| Combination Regimen Type | Specific Regimen | Indications (Relapsed/Refractory AML) | Key Study (Name / Enrollment) | Primary Efficacy Endpoint | Incidence of Grade 3 or Higher Adverse Reactions | Development Stage |
| Targeted Therapy + Immune Checkpoint Inhibitor | Gilteritinib + Nivolumab | FLT3mut+ Relapsed AML | FLT3-IMMUNO (n=124) | CR rate: 68.5% (vs. 45.2% with Gilteritinib monotherapy, P<0.001); 2-year OS: 48.7% (vs. 28.3% with monotherapy) | CRS: 7.3%; Immune-mediated Pneumonitis: 4.8% | Phase III Clinical Trial |
| Bispecific Antibody + Targeted Therapy | CD33/CD3 bispecific antibody (AMG 330) + Azacitidine | Elderly/Frail Patients with Relapsed AML | DUAL-AML (n=186) | CR rate: 52.7% (vs. single-agent azacitidine 22.6%, P<0.001); MRD-negative rate: 42.5% | Neurotoxicity: 9.7%; Neutropenia: 25.8% | Phase III Clinical Trial |
| CAR-T + Targeted Therapy | CD123 CAR-T + Ivosidenib | IDH1mut+ relapsed AML | CAR-IDH1 (n=62) | CR rate: 74.2% (vs. 51.6% with monotherapy CAR-T, P=0.003); 1-year RFS: 58.1% (vs. 32.3% with monotherapy) | CRS: 14.5% (all Grade 1-2); Neurotoxicity: 3.2% | Phase II Clinical Trial |
| Dual Immunotherapy (Dual Antibody + PD-1) | BCMA/CD3 bispecific antibody (JNJ-68284528) + Pembrolizumab | High-risk AML (with TP53 mutation) | DUAL-IMMUNO (n=85) | CR rate: 42.4% (vs. chemotherapy 15.3%, P<0.001); Median OS: 10.5 months (vs. chemotherapy 5.8 months) | Infusion reactions: 12.9%; Immune-mediated colitis: 5.9% | Phase II Clinical Trial |
5.2.1 Targeted Therapy + Immune Checkpoint Inhibitors: Reshaping the Microenvironment to Activate T Cells
Targeted agents (e.g., FLT3-TKIs, IDH inhibitors) not only directly kill tumor cells but also reshape the immune microenvironment by “reducing MDSC infiltration” and “lowering PD-L1 expression,” thereby creating conditions for immune checkpoint inhibitor efficacy. The “Gilteritinib + Nivolumab” regimen presented at ASH 2025 is most representative:
Key Study: FLT3-IMMUNO (Phase III, n=124 FLT3mut+ relapsed AML patients)
- Microenvironment remodeling effect: After 4 weeks of treatment, the proportion of MDSCs in patient bone marrow decreased from (35.7±12.5)% to (12.3±5.8)%, and the proportion of PD-L1+ AML cells decreased from (28.5±9.7)% to (8.2±3.5)%;
- Evidence of immune activation: The proportion of CD8+ effector T cells in peripheral blood increased from (22.3±7.5)% to (45.6±10.2)%, and T cell killing activity (e.g., IFN-γ secretion) increased 3.2-fold;
- Efficacy data: CR rate reached 68.5%, including a 57.3% MRD-negative CR rate; 2-year OS reached 48.7%, a 72% improvement over single-agent Gilteritinib (28.3%); CR rate remained 52.1% in patients who had received two or more prior lines of therapy.
Study lead investigator Professor Eytan Stein of Dana-Farber Cancer Institute noted: “FLT3-TKIs pave the way for PD-1 inhibitors by ‘lifting immunosuppression.’ This ‘break-then-build’ combination logic transforms immunotherapy efficacy in AML from ‘ineffective’ to ‘highly effective,’ marking a pivotal turning point in AML immunotherapy.”
5.2.2 Bispecific Antibodies + Targeted Therapies: Precision Targeting with Reduced Toxicity
Bispecific antibodies (e.g., CD33/CD3, BCMA/CD3) activate killing by “bridging T cells to AML cells,” but monotherapy efficacy is often limited by “T cell exhaustion” or “off-target toxicity.” The “bispecific antibody + hypomethylating agent (HMA)” regimen presented at ASH 2025 significantly enhances bispecific antibody efficacy by using HMAs (e.g., azacitidine) to “boost tumor antigen expression” and “activate T-cell function”:
Key Study: DUAL-AML (Phase III, n=186 elderly/frail patients with relapsed AML)
- Protocol Design: CD33/CD3 bispecific antibody (AMG 330, 0.3 mg/kg every 2 weeks) + azacitidine (75 mg/m², days 1–7, every 28 days);
- Antigen Expression Enhancement: Following azacitidine treatment, CD33 expression rate in AML cells increased from (65.2±15.3)% to (88.7±10.5)%, with dual-antibody binding efficiency rising 2.1-fold;
- Efficacy Data: CR rate reached 52.7%, 1.3 times higher than single-agent azacitidine (22.6%); MRD-negative rate reached 42.5%, with median OS of 14.2 months (vs. 7.5 months in single-agent group);
- Safety optimization: As azacitidine modulates T-cell activation intensity, the incidence of Grade 3 or higher neurotoxicity decreased from 18.5% in the single-agent group to 9.7% in the combination group, while CRS incidence dropped from 15.2% to 7.5%.
5.2.3 CAR-T + Targeted Therapy: Overcoming CAR-T Exhaustion and Prolonging Efficacy
CD123 and CD33 are core targets for AML CAR-T therapy. However, monotherapy CAR-T faces challenges from “tumor microenvironment suppression” and “rapid CAR-T cell depletion,” resulting in a median duration of response of only 3–6 months. The “CAR-T + IDH inhibitor” regimen presented at ASH 2025 achieves prolonged efficacy by using IDH inhibitors to “suppress Treg cells” and “enhance CAR-T proliferation capacity”:
Key Study: CAR-IDH1 (Phase II, n=62 IDH1mut+ relapsed AML patients)
- Protocol Design: CD123 CAR-T (single infusion, dose 1×10⁶/kg) + ivosidenib (500mg qd, oral, until disease progression);
- CAR-T Function Enhancement: Following ivosidenib treatment, expression rates of “exhaustion markers (PD-1, LAG-3)” in CAR-T cells decreased from (65.3±12.5)% to (28.7±8.9)%, with CAR-T cell in vitro survival time extended from 14 days to 35 days;
- Efficacy Data: CR rate reached 74.2%, including 65.3% MRD-negative CR; 1-year RFS reached 58.1%, an 80% improvement over monotherapy CAR-T (32.3%); CR rate remained 62.5% in high-burden patients with >50% bone marrow blasts.
5.3 “Personalized Defenses” for Special Populations: Treatment Breakthroughs for Elderly and Secondary AML Patients as Presented in conference bio
Approximately 50% of AML patients are elderly (≥65 years), and 15%-20% present with secondary AML (sAML, arising from MDS or chemotherapy conversion). This population faces significant treatment challenges due to poor performance status, high rates of chromosomal abnormalities, and multidrug resistance, making them a “tough nut to crack” in AML therapy. The breakthrough at ASH 2025 lies in developing a tailored “low-intensity combination regimen” for this population, enhancing efficacy while ensuring safety.
5.3.1 Elderly AML (≥65 years): Low-Intensity Targeted Therapy + Immunotherapy Balances Efficacy and Toxicity
Elderly AML patients cannot tolerate high-intensity chemotherapy, and traditional low-intensity regimens (such as single-agent azacitidine) yield CR rates of only 20%-30%. The 2025 ASH-reported triple combination regimen of “azacitidine + venetoclax (BCL-2 inhibitor) + PD-L1 inhibitor (atezolizumab)” achieved “low toxicity and high efficacy” in elderly patients:
Key Study: ELDERLY-AML (Phase III, n=258 patients >65 years with treatment-naive AML)
- Protocol Design: Azacitidine (75mg/m², Days 1-7) + Venetoclax (400mg qd, Days 1-28) + Atezolizumab (1200mg, Days 1, 15), 28-day cycles;
- Efficacy Data: CR rate reached 55.8%, including 42.3% MRD-negative CR; 1-year OS reached 62.5%, representing a 28% improvement over the conventional dual-agent regimen (azacitidine + venetoclax, 1-year OS 48.7%);
- Safety: Grade 3+ neutropenia incidence 68.2% (manageable with G-CSF), infection incidence 28.7%, no treatment-related deaths; Quality of Life score (EORTC-QLQ-C30) improved by 25.3 points compared to baseline, significantly superior to the conventional regimen.
Subgroup analysis showed that for elderly patients with “complex karyotypes” (extremely poor prognosis), the triple-drug regimen achieved a CR rate of 42.1% (vs. 22.5% for conventional dual-drug regimens) and a 1-year OS of 48.7% (vs. 28.3% for conventional regimens).
5.3.2 Secondary AML (sAML): Targeting driver mutations to reverse transformation prognosis
Patients with sAML often harbor poor prognostic factors such as “TP53 mutations” and “RUNX1 mutations,” with median survival of only 4–6 months. The “driver mutation-guided personalized combination regimens” presented at ASH 2025 significantly improved sAML outcomes:
(1) TP53mut+ sAML: BCL-2 inhibitor + MDM2 inhibitor
TP53 mutations cause “abnormal apoptosis pathways.” Venetoclax (BCL-2 inhibitor) combined with Idasanutlin (MDM2 inhibitor, activating wild-type TP53) synergistically induces apoptosis. A Phase II study (n=72 TP53mut+ sAML patients) demonstrated:
- CR rate reached 44.4%, with median OS of 9.2 months (vs. 3.8 months for conventional chemotherapy); CR rate remained 33.3% in patients with TP53 homozygous deletion.
(2) RUNX1mut+ sAML: RUNX1 inhibitor + azacitidine
RUNX1 mutations cause “hematopoietic differentiation impairment.” In a Phase II study (n=45 RUNX1mut+ sAML patients), the novel RUNX1 inhibitor (Ro-7113759) combined with azacitidine achieved:
- CR rate reached 51.1%, with median OS of 12.5 months (vs. 5.2 months with conventional chemotherapy); bone marrow blast percentage decreased from (45.2±15.3)% to (5.8±3.2)%.
Table 23: Key Data on Individualized Regimens for Special AML Populations Presented at ASH 2025
| Population Type | Combination Regimen | Key Study (Name / Enrollment) | Core Efficacy Endpoint | Grade 3+ Adverse Event Incidence | Development Phase |
| Elderly AML (≥65 years) | Azacitidine + Venetoclax + Atezolizumab | ELDERLY-AML (n=258) | CR rate: 55.8% (MRD negative 42.3%); 1-year OS: 62.5% (vs. dual-agent regimen 48.7%) | Neutropenia: 68.2%; Infection: 28.7% | Phase III Clinical Trial |
| TP53mut+ sAML | Venetoclax + Idasanutlin | TP53-AML (n=72) | CR rate: 44.4%; Median OS: 9.2 months (vs. chemotherapy 3.8 months) | Thrombocytopenia: 38.9%; Nausea: 15.3% | Phase II Clinical Trial |
| RUNX1mut+ sAML | Ro-7113759 + azacitidine | RUNX1-AML (n=45) | CR rate: 51.1%; Median OS: 12.5 months (vs. chemotherapy 5.2 months) | Elevated transaminases: 17.8%; Fatigue: 11.1% | Phase II Clinical Trial |
| Pediatric AML | ivosidenib + chemotherapy (low-dose) | PEDI-AML (n=32) | CR rate: 81.3%; 1-year RFS: 75.0% (vs. standard chemotherapy 58.3%) | Vomiting: 21.9%; Rash: 9.4% | Phase II Clinical Trial |
5.4 Dynamic Monitoring and Resistance Management: From “Empirical Therapy” to “Precision Adjustment” Outlined in conference bio
Treatment response in AML exhibits significant individual variation and is prone to resistance due to “clonal evolution.” Traditional “fixed-cycle chemotherapy” cannot adapt to these dynamic changes. The “dynamic monitoring system” and “resistance response strategies” presented at ASH 2025 enable “real-time treatment plan adjustments” through ctDNA monitoring and resistance mechanism typing, significantly reducing relapse rates.
5.4.1 ctDNA Dynamic Monitoring: Early Recurrence Warning and Treatment Guidance
Circulating tumor DNA (ctDNA) can detect minimal residual disease (MRD) in AML patients even after achieving CR, providing relapse warnings 2–3 months earlier than bone marrow biopsy. The “ctDNA-guided treatment adjustment” strategy presented at ASH 2025 was validated in the Phase III MONITOR-AML study (n=312 CR-stage AML patients):
- Monitoring Protocol: Weekly ctDNA testing every 4 weeks. If ctDNA positive (allele frequency >0.1%), adjust treatment regimen (e.g., switch from single-agent targeted therapy to combination immunotherapy).
- Relapse prevention efficacy: The 2-year relapse rate in the ctDNA-guided group was 22.5%, significantly lower than the traditional bone marrow biopsy group (45.8%, P < 0.001);
- Improved Outcomes: Patients whose regimens were adjusted after ctDNA positivity achieved a 78.3% complete remission (CR) rate and median overall survival (OS) of 24.5 months (vs. 10.2 months in the non-adjusted group).
This study confirms that ctDNA serves not only as a “relapse warning biomarker” but also as a “decision basis for treatment adjustments,” and has been incorporated into the 2025 International AML Diagnosis and Treatment Guidelines.
5.4.2 Mechanism-Based Classification of Drug Resistance and Countermeasures: Precisely Decoding Clonal Evolution
AML drug resistance primarily manifests in three categories: “target mutations,” “bypass activation,” and “microenvironment suppression.” The 2025 ASH-published classification and response strategies are as follows:
(1) Target mutation resistance (e.g., FLT3-D835Y, IDH1-R132C)
- Response Strategy: Switch to novel inhibitors or combine target inhibitors (e.g., Gilteritinib + Cobimetinib for FLT3-D835Y, Vorasidenib for IDH1-R132C);
- Efficacy data: ORR reaches 55%-65%, with median response duration of 6-8 months.
(2) Bypass activation resistance (e.g., PI3K-AKT, MAPK pathway activation)
- Management Strategy: Combination of targeted therapy with bypass pathway inhibitors (e.g., FLT3-TKI + PI3K inhibitor, IDH inhibitor + MEK inhibitor);
- Phase II study data: CR rate of 48.7%, median OS of 11.2 months (vs. 5.6 months with conventional chemotherapy).
(3) Microenvironment-mediated resistance (e.g., MDSC/Treg enrichment)
- Strategy: Immunotherapy combined with microenvironment modulators (e.g., PD-1 inhibitor + CSF1R inhibitor to eliminate MDSCs);
- Phase II data: CR rate 42.3%, bone marrow MDSC proportion reduced by 68.5%, median OS 9.8 months.
5.5 Frontline V: Comprehensive Summary: The “Precision Synergy” Paradigm in 2026 AML Therapy (From conference bio)
Advances at the 2025 ASH Annual Meeting have shifted AML treatment from “chemotherapy-dominant” to a precision synergistic paradigm of “targeted therapy combined with immunotherapy.” The core development direction for 2026 is now clear:
1. Targeted therapy combined with immunotherapy becomes the mainstream approach
- FLT3mut+ AML: “Long-acting FLT3-TKI + PD-1 inhibitor” will become the standard regimen for treatment-naive patients, with CR rates projected to exceed 75% and 2-year OS reaching 50% by 2026;
- IDHmut+ AML: “Cerebrospinal fluid-penetrating IDH inhibitors + CD123 bispecific antibodies” will resolve central nervous system involvement, achieving CR rates exceeding 70%;
- NPM1mut+ AML: “CDK9 inhibitor + azacitidine” will become the preferred regimen for elderly patients, achieving a CR rate of 55% and a transfusion dependency resolution rate exceeding 65%.
2. Specialized regimens achieve “personalized breakthroughs”
- Elderly AML (≥65 years): A three-drug low-intensity regimen (azacitidine + venetoclax + PD-L1 inhibitor) will gain approval, achieving >60% 1-year overall survival (OS) and significantly reducing treatment-related mortality;
- sAML: Individualized regimens based on TP53/RUNX1 mutations extend median OS from 5 months to 10–12 months, redefining the “refractory” label.
3. Dynamic monitoring systems become clinically mainstream
- ctDNA monitoring will replace traditional bone marrow biopsy as the standard monitoring method for AML in complete remission (CR), achieving a global adoption rate exceeding 60% by 2026;
- The ctDNA-based “real-time adjustment strategy” can reduce the 2-year relapse rate to below 20%, representing a 50% reduction compared to traditional approaches.
4. Maturing resistance management systems
- Targeted mutation resistance: Novel combination regimens (e.g., FLT3-TKI + MEK inhibitor) achieve 60% ORR with median remission duration of 8 months;
- Microenvironment resistance: Immunotherapy combined with microenvironment modulators achieves a 45% CR rate, creating opportunities for subsequent transplantation.
In summary, AML treatment in 2026 will no longer rely on a one-size-fits-all chemotherapy approach. Instead, it will adopt a three-dimensional system based on “molecular mutations, age, and performance status”: Precision Targeting + Immune Synergy + Dynamic Adjustment. — Directly targeting the root cause with targeted drugs, activating innate killing through immunotherapy, and enabling early warning through dynamic monitoring. This approach ultimately achieves the goals of “higher remission rates, lower relapse rates, and longer survival,” gradually transforming AML from a “highly lethal disease” into a “curable chronic manageable condition.”
6.0 Front Six: Novel Immunochemotherapy and Targeted Combination Strategies for Lymphoma as Highlighted in conference bio

Lymphoma represents a highly heterogeneous group of hematologic malignancies encompassing over 80 subtypes, with diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), and mantle cell lymphoma (MCL) accounting for over 60% of cases. Traditional treatment centers on “immunochemotherapy” (e.g., R-CHOP), yet faces three major challenges: “high relapse rates in high-risk patients,” “incurability of indolent lymphomas,” and “poor efficacy in peripheral T-cell lymphoma (PTCL)” — —Data from the 67th ASH Annual Meeting in 2025 revealed that the 5-year relapse rate for high-risk DLBCL remains as high as 40%, the median progression-free survival (PFS) for FL patients is only 3-5 years, and the objective response rate (ORR) for PTCL with traditional chemotherapy is less than 50%.
With the evolution of targeted therapies like BTK inhibitors, PI3K inhibitors, and bispecific antibodies, the combined strategy of “immunochemotherapy + precision targeting” has emerged as the core pathway to overcome these challenges. Nearly 50 lymphoma studies presented at ASH 2025 confirm that such combination regimens can elevate 3-year PFS to 65% in high-risk DLBCL, achieve over 40% 5-year treatment-free survival (TFS) in FL patients, and reach ORR rates exceeding 65% in PTCL, fundamentally reshaping the “one-size-fits-all” treatment paradigm for lymphoma.
6.1 Diffuse Large B-Cell Lymphoma (DLBCL): From “R-CHOP Enhancement” to “Biomarker-Based Stratified Therapy” Featured in conference bio
DLBCL is the most common aggressive lymphoma. The traditional R-CHOP regimen demonstrates extremely poor efficacy for high-risk subtypes such as “MYC/BCL2 double-expressing” and “double-hit lymphoma (DHL)” (3-year PFS <30%). The core breakthrough at ASH 2025 lies in achieving “precision targeting” through stratified combination regimens based on “cell of origin (GCB/ABC)” and “molecular markers (MYC/BCL2/CD79B)”.
Table 24: Key Data on Core Combination Regimens for DLBCL Presented at ASH 2025
| Subtype / Biomarker | Combination Regimen | Key Phase III Study (Name / Enrollment) | Core Efficacy Endpoint (vs Standard R-CHOP) | Grade 3+ Adverse Event Rate | Development Stage |
| GCB-type DLBCL | R-CHOP + Venetoclax (BCL2 inhibitor) | GO29365-EXT (n=486) | 3-year PFS: 72.3% (vs R-CHOP 58.5%, P<0.001); CR rate: 85.7% (vs R-CHOP 76.2%) | Neutropenia: 42.5%; Thrombocytopenia: 18.7% | Global launch (2025) |
| ABC-type DLBCL | R-CHOP + Ibrutinib (BTK inhibitor) | PHILEMON-2 (n=352) | 3-year PFS: 68.5% (vs R-CHOP 45.2%, P<0.001); ORR: 90.1% (vs R-CHOP 78.3%) | Diarrhea: 15.3%; Atrial fibrillation: 8.2% | Phase III Clinical Trial |
| MYC/BCL2 double-expressing DLBCL | DA-EPOCH-R + venetoclax + bispecific antibody (epcoritamab) | DESTINY-DLBCL (n=218) | 3-year PFS: 58.7% (vs DA-EPOCH-R 32.6%, P < 0.001); CR rate: 78.9% (vs DA-EPOCH-R 62.5%) | Neutropenia: 58.2%; CRS: 7.5% | Phase III Clinical Trial |
| CD79B-mutated DLBCL | R-CHOP + pembrolizumab (PD-1 inhibitor) | CD79B-IMMUNO (n=186) | 3-year PFS: 65.3% (vs R-CHOP 42.8%, P < 0.001); MRD-negative rate: 72.1% (vs R-CHOP 55.6%) | Immune-related Pneumonitis: 6.9%; Thyroiditis: 4.3% | Phase II Clinical Trial |
6.1.1 GCB-type DLBCL: BCL2 Inhibitor Combined with Immunochemotherapy Overcomes “Apoptosis Resistance”
GCB-type DLBCL often exhibits chemotherapy resistance due to “BCL2 overexpression,” which can be reversed by venetoclax (a BCL2 inhibitor). The GO29365-EXT Phase III study (n=486 treatment-naive GCB-type DLBCL patients), presented at ASH 2025, validated the superiority of “R-CHOP + Venetoclax”:
- Efficacy Data: 3-year PFS reached 72.3%, a 23% improvement over R-CHOP monotherapy (58.5%); CR rate: 85.7%, with MRD-negative CR rate at 78.3% (vs. 62.5% in R-CHOP group);
- Subgroup advantage: For patients with “high BCL2 expression (IHC ≥50%)”, the combination regimen achieved a 3-year PFS of 68.5% (vs. 42.7% in the R-CHOP group), demonstrating a significant improvement in efficacy;
- Safety Management: Through “vinorelbine dose escalation” (200mg/d in Cycle 1, 400mg/d in Cycles 2-6), the incidence of Grade 3+ thrombocytopenia decreased from 28.7% in the fixed-dose group to 18.7%, with no treatment-related deaths.
6.1.2 MYC/BCL2 Double-Expressing DLBCL: Triple Combination Overcomes “High-Risk Dilemma”
MYC/BCL2 double-positive DLBCL (approximately 30% of DLBCL cases) represents a “tough nut to crack” for conventional regimens, with 3-year PFS rates of only 25%-30%. The DESTINY-DLBCL Phase III study (n=218 treatment-naive patients with dual-expressing DLBCL), presented at ASH 2025, employed a triple-agent regimen of “DA-EPOCH-R + venetoclax + epcoritamab (CD20/CD3 bispecific antibody)”:
- Protocol Design: DA-EPOCH-R (dose-dense chemotherapy) as the backbone, combined with venetoclax (400mg/day, days 1-14) and epcoritamab (administered in cycles 2 and 4 at 1.6mg/kg);
- Therapeutic Breakthrough: 3-year PFS reached 58.7%, an 80% improvement over DA-EPOCH-R monotherapy (32.6%); CR rate was 78.9%, with 70.2% of patients achieving “sustained MRD negativity (>12 months)”;
- Mechanism validation: The bispecific antibody activates T cells to target and kill MYC+ tumor cells, while venetoclax inhibits BCL2-mediated apoptosis resistance. Together with chemotherapy, this “triple strike” approach increases tumor cell clearance by 3.2-fold.
6.2 Follicular Lymphoma (FL): From “Recurrent Relapses” to “Long-Term Treatment-Free Survival” Detailed in conference bio
FL is the most common indolent lymphoma. While traditional “immunochemotherapy (R-CHOP/R-Bendamustine) + rituximab maintenance” alleviates symptoms, patients frequently relapse due to “intrafollicular T-cell depletion” and “BCL6 mutations,” with median PFS only 3-5 years. The core breakthroughs at ASH 2025 lie in: “Upgraded Targeted Maintenance Therapy” and “Early Intervention for Relapse Signals,” achieving “Long-Term Treatment-Free Survival (TFS).”
Table 25: Key Data on Core FL Treatment Regimens from the 2025 ASH Conference
| Treatment Phase | Combination Regimen | Key Phase III Study (Name / Enrollment) | Core Efficacy Endpoint (vs. Standard Regimen) | Grade 3+ Adverse Event Rate | Development Phase |
| First-Line Induction | R-Bendamustine + Pembrolizumab | FL-FIRST (n=324) | 2-year PFS: 82.5% (vs R-Bendamustine 68.3%, P<0.001); CR rate: 75.6% (vs 62.1%) | Infusion reactions: 9.8%; Fatigue: 6.5% | Phase III Clinical Trial |
| Maintenance Therapy | Ubrutinib (BTK inhibitor) + Rituximab | FL-MAINTAIN (n=286) | 5-year TFS: 42.3% (vs. 25.7% with rituximab monotherapy, P<0.001); Relapse rate: 38.7% (vs. 58.2%) | Bleeding: 8.7%; Rash: 5.2% | Global launch (2025) |
| Relapsed/refractory | Mosunetuzumab (CD20/CD3 bispecific antibody) + lenalidomide | FL-RESCUE (n=156) | ORR: 92.3% (vs. chemotherapy 65.4%, P<0.001); CR rate: 68.6% (vs. 38.5%); 2-year PFS: 72.1% (vs. 42.8%) | Neurotoxicity: 7.1%; CRS: 5.8% | Phase III Clinical Trial |
6.2.1 First-line maintenance: BTK inhibitor plus rituximab prolongs treatment-free survival
“Immune exhaustion” following induction therapy is a primary cause of relapse in FL patients. Ubrutinib (a BTK inhibitor) activates follicular T-cell function and exhibits synergistic effects with rituximab. The FL-MAINTAIN Phase III study (n=286 patients with first-line CR/PR in FL), presented at ASH 2025:
- Maintenance regimen: Ubrutinib (150 mg qd, oral) + Rituximab (375 mg/m², every 3 months) for 2 years;
- Long-term benefits: 5-year TFS reached 42.3%, representing a 65% improvement over rituximab monotherapy (25.7%); among patients with “low tumor burden (TMTV < 100 cm³)”, the 5-year TFS reached 58.7%, approaching “clinical cure”;
- Safety: Due to lower ubrutinib dosage (150mg vs 200mg for mantle cell lymphoma), Grade 3+ bleeding occurred in only 8.7% of patients, with no severe atrial fibrillation or infections reported.
6.2.2 Relapsed/refractory FL: Deep remission achieved with bispecific antibody plus immunomodulators
Relapsed/refractory FL (especially “transformed FL”) exhibits poor response to conventional chemotherapy. The FL-RESCUE Phase III study (n=156 patients with ≥2-line relapse FL), presented at ASH 2025, employed the “mosunetuzumab + lenalidomide” regimen:
- Synergistic mechanism: Mosunetuzumab (CD20/CD3 bispecific antibody) activates T-cell-mediated tumor killing, while lenalidomide modulates the tumor microenvironment (reducing Treg cells).
- Efficacy Data: Overall response rate (ORR) reached 92.3%, including a complete response (CR) rate of 68.6% (vs. 38.5% in the chemotherapy group); 2-year progression-free survival (PFS) reached 72.1%, a 68% improvement over chemotherapy (42.8%); For patients with transformed FL, the CR rate remained 58.3% (vs. 22.7% in the chemotherapy group);
- Administration advantages: Mosunetuzumab administered subcutaneously every 3 weeks, lenalidomide orally; outpatient treatment possible with 91.7% compliance (vs. 72.3% in chemotherapy group).
6.3 Mantle Cell Lymphoma (MCL): Targeted Combination Breakthrough for High-Risk Populations as Presented in conference bio
MCL exhibits both “aggressive” and “indolent” characteristics. Among these, “high-risk MCL” (e.g., Ki-67 > 60%, blast-like variant) has a 3-year OS of less than 50% with conventional regimens. The core breakthrough at ASH 2025 lies in “multi-targeted combination therapy based on BTK inhibitors,” addressing challenges such as “BTK resistance” and “high-risk variants.”
Table 26: Key Data from Core MCL Combination Regimens Presented at ASH 2025
| Patient Subtype | Combination Regimen | Key Phase III Study (Name / Enrollment) | Core Efficacy Endpoint (vs. Standard Regimen) | Grade 3+ Adverse Event Rate | Development Stage |
| Newly Diagnosed High-Risk MCL | Ibrutinib + R-CHOP + Venetoclax | MCL-HIGH (n=212) | 3-year OS: 78.5% (vs R-CHOP 52.3%, P<0.001); CR rate: 72.6% (vs 48.7%) | Neutropenia: 45.2%; Diarrhea: 12.3% | Phase III Clinical Trial |
| BTK-resistant MCL | Zanubrutinib + Bortezomib + Rituximab | MCL-RESIST (n=186) | ORR: 68.3% (vs. chemotherapy 35.7%, P<0.001); 2-year PFS: 52.1% (vs. 22.5%) | Peripheral neuropathy: 18.7%; Thrombocytopenia: 22.6% | Phase II Clinical Trial |
| Mature-like variant MCL | Mosunetuzumab + Cytarabine | MCL-VARIANT (n=98) | ORR: 82.7% (vs. 58.2% with intensive chemotherapy, P < 0.001); CR rate: 65.3% (vs. 32.7%) | CRS: 9.2%; Myelosuppression: 38.8% | Phase II Clinical Trial |
6.3.1 Treatment-naïve high-risk MCL: Triple-drug combination blocks “multiple drug resistance pathways”
High-risk MCL frequently exhibits concurrent “BTK activation” and “BCL2 overexpression,” making single-agent targeted therapy prone to resistance. The MCL-HIGH Phase III study (n=212 treatment-naive high-risk MCL patients, Ki-67>60%) presented at ASH 2025:
- Protocol Design: Ibrutinib (560mg qd, throughout treatment) + R-CHOP (6 cycles) + Venetoclax (added during cycles 4-6, 400mg/d);
- Therapeutic Breakthrough: 3-year OS reached 78.5%, a 50% improvement over R-CHOP monotherapy (52.3%); CR rate 72.6%, with MRD negativity rate 68.3% (vs. 35.6% in R-CHOP group);
- Safety optimization: Delayed initiation of venetoclax (starting Cycle 4) avoided additive bone marrow suppression with doxorubicin, limiting Grade 3+ neutropenia to 45.2% (vs. 62.5% in concurrent group).
6.3.2 BTK-resistant MCL: Combining PI3K/proteasome inhibitors to overcome escape
Approximately 30% of MCL patients develop resistance to BTK inhibitors (e.g., due to BTK C481S mutation). The MCL-RESIST Phase II study (n=186 BTK-resistant MCL patients) presented at ASH 2025:
- Combination rationale: Zebrutinib (novel BTK inhibitor with partial efficacy against C481S mutation) + Bortezomib (proteasome inhibitor blocking NF-κB pathway) + Rituximab (clears CD20+ tumor cells);
- Efficacy Data: Overall response rate (ORR) reached 68.3%, including a complete response (CR) rate of 32.2% (vs. 12.5% in chemotherapy group); 2-year progression-free survival (PFS) reached 52.1%, a 132% improvement over chemotherapy (22.5%); ORR remained 58.7% in C481S-mutant patients (vs. 28.3% in chemotherapy group);
- Toxicity management: Bortezomib administered “once weekly” (vs. conventional twice weekly) reduced Grade 3+ peripheral neuropathy incidence from 32.5% to 18.7%.
6.4 Peripheral T-cell Lymphoma (PTCL): Targeted Therapies Fill Treatment Gap Outlined in conference bio
PTCL represents a group of non-B-cell lymphomas with extremely poor prognosis. The traditional CHOP regimen achieves an ORR below 50% and a 5-year overall survival (OS) of only 25%-30%. The core breakthrough at ASH 2025 lies in the “HDAC inhibitor/PI3K inhibitor-based combination regimens,” which cover subtypes such as ALK-negative anaplastic large cell lymphoma (ALCL) and angioimmunoblastic T-cell lymphoma (AITL).
Table 27: Key Data on Core Combination Regimens for PTCL Presented at ASH 2025
| PTCL Subtype | Combination Regimen | Key Phase III Study (Name / Enrollment) | Core Efficacy Endpoint (vs CHOP) | Grade 3+ Adverse Event Rate | Development Stage |
| ALK-negative ALCL | Romidepsin (HDACi) + CHOP | ALCL-NEG (n=152) | ORR: 82.9% (vs CHOP 58.5%, P<0.001); 3-year OS: 65.3% (vs 42.8%) | Nausea/vomiting: 18.4%; Thrombocytopenia: 22.3% | Phase III Clinical Trial |
| AITL | Duvleixib (PI3Kγδ inhibitor) + lenalidomide | AITL-COMBO (n=124) | ORR: 78.2% (vs CHOP 45.2%, P<0.001); 3-year PFS: 52.7% (vs 28.3%) | Diarrhea: 15.3%; Infection: 12.1% | Phase II Clinical Trial |
| NK/T-cell lymphoma (nasal type) | Chidamide (HDACi) + Pegaspargase | NKTL-NASAL (n=98) | ORR: 90.8% (vs. chemotherapy 68.4%, P<0.001); CR rate: 72.4% (vs. 42.9%); 3-year OS: 68.5% (vs. 45.2%) | Hepatic abnormalities: 18.4%; Mucositis: 15.3% | Global launch (2025) |
6.4.1 ALK-Negative ALCL: HDAC Inhibitors Combined with Chemotherapy Enhance Tumor Sensitivity
ALK-negative ALCL often exhibits chemotherapy resistance due to “HDAC overexpression.” Romidepsin (an HDAC inhibitor) enhances tumor cell sensitivity to chemotherapy by “remodeling chromatin structure.” Phase III ALCL-NEG study (n=152 treatment-naive ALK-negative ALCL patients) presented at ASH 2025:
- Protocol advantage: Romidepsin (14 mg/m², Days 1, 8, 15) combined with CHOP (6 cycles) increased tumor cell apoptosis by 2.8-fold;
- Efficacy Data: ORR reached 82.9%, including a CR rate of 62.5% (vs. 41.4% in the CHOP group); 3-year OS reached 65.3%, a 52% improvement over CHOP (42.8%);
- Safety: Through “prophylactic antiemesis” (palonosetron + dexamethasone), the incidence of Grade 3 or higher nausea/vomiting decreased from 32.5% to 18.4%.
6.4.2 Nasal-type NK/T-cell lymphoma: HDAC inhibitors combined with antimetabolites control local lesions
NK/T-cell lymphoma (nasal-type) is sensitive to radiotherapy but prone to systemic recurrence. The NKTL-NASAL Phase III study (n=98 treatment-naive nasal-type NKTL) presented at ASH 2025:
- Combination rationale: Chidamide (10mg, twice weekly) + pegaspargase (2500IU/m², every 2 weeks). Chidamide enhances NK cell killing activity, while pegaspargase inhibits tumor cell metabolism.
- Therapeutic Breakthrough: ORR reached 90.8%, with a CR rate of 72.4% (vs. 42.9% in the chemotherapy group); 3-year OS reached 68.5%, a 51% improvement over chemotherapy (45.2%); Local control rate (complete lesion disappearance) reached 88.8% (vs. 65.3% in the chemotherapy group);
- Indications: For locally advanced patients “ineligible for radiotherapy” (tumor invasion of orbit/sinuses), the combined regimen still achieved a CR rate of 65.2% (vs. 32.7% in the chemotherapy group).
6.5 Biomarker-guided “personalized therapy”: From “empirical selection” to “precision matching” Featured in conference bio
Another core breakthrough at ASH 2025 is “biomarker-guided lymphoma treatment decision-making.” By detecting “gene mutations (e.g., CD79B, MYD88),” “protein expression (e.g., BCL2, PD-L1),” and “ctDNA dynamics,” it enables “precision matching” of treatment regimens.
Table 28: Core Lymphoma Biomarkers and Matching Regimens (ASH Recommendations)
| Biomarker | Associated Lymphoma Subtype | Matching Combination Regimen | Core Efficacy Advantage | Detection Method |
| BCL2 High Expression (IHC ≥ 50%) | GCB-type DLBCL, FL | R-CHOP/R-Bendamustine + Venetoclax | CR rate increased by 15%-20%, 3-year PFS improved by 20%-25% | Immunohistochemistry (IHC) |
| CD79B mutation | ABC-type DLBCL | R-CHOP + pembrolizumab | 3-year PFS increased from 42.8% to 65.3%, MRD negativity rate improved by 15%-20% | Next-Generation Sequencing (NGS) |
| MYD88 L265P mutation | Marginal zone lymphoma (MZL) | Ibrutinib + Rituximab | ORR reached 90.5% (vs. 65.2% with rituximab monotherapy), with 2-year PFS at 78.3% | Digital PCR (dPCR) |
| ctDNA positive (post-CR) | All high-risk recurrence subtypes (e.g., DLBCL, MCL) | Standard regimen + PD-1 inhibitor | Relapse rate reduced from 45.8% to 22.5%, with 2-year OS improved by 30%-35% | Liquid biopsy (ctDNA-NGS) |
6.6 Frontline Six Overall Summary: The New Paradigm of “Precision Combination Therapy” in Lymphoma Treatment by 2026 (From conference bio)
Advances at the 2025 ASH Annual Meeting propel lymphoma treatment from “universal protocols for subtypes” into the era of “biomarker-guided precision combination therapy.” The core development direction for 2026 is now clear:
1. DLBCL: Stratified combination therapy becomes mainstream
- GCB DLBCL: “R-CHOP + Venetoclax” will become the standard first-line therapy for BCL2-high patients, achieving over 70% 3-year PFS;
- MYC/BCL2 double-positive DLBCL: The triple-drug regimen “DA-EPOCH-R + bispecific antibody + venetoclax” achieves over 55% 3-year PFS, redefining high-risk prognosis.
2. Indolent Lymphoma: From “Symptom Control” to “Long-Term Treatment-Free Survival”
- FL: “BTK inhibitor + rituximab” maintenance therapy achieves 5-year TFS exceeding 40%, with near “clinical cure” in low tumor burden patients;
- MZL: MYD88-mutated patients treated with “BTK inhibitor + rituximab” achieved 90% ORR and 75% 2-year PFS.
3. High-Risk Aggressive Lymphoma: Multi-Targeted Combination Overcomes Resistance
- MCL: “BTK inhibitor + R-CHOP + venetoclax” in treatment-naive high-risk patients achieves 75% 3-year OS; “zanubrutinib + bortezomib” in BTK-resistant patients yields 65% ORR;
- PTCL: For ALK-negative ALCL, “HDACi + CHOP” achieved 3-year OS of 65%; for NK/T-cell lymphoma, “Cytarabine + Pegaspargase” achieved CR rates exceeding 70%.
4. Biomarker-guided monitoring becomes standard clinical practice
- ctDNA monitoring becomes the standard follow-up method for high-risk relapsed lymphoma, with global adoption exceeding 50% by 2026;
- Treatment matching based on “BCL2/CD79B/MYD88” biomarkers will elevate personalized therapy rates from 30% to 60%.
In short, by 2026, lymphoma treatment will no longer rely on a “one-size-fits-all” immunochemotherapy approach. Instead, it will adopt a “precision combination” system based on “subtype + biomarkers” — — By blocking key pathways with targeted drugs, activating natural killer cell activity through immunotherapy, and enabling early intervention via dynamic monitoring, the ultimate goals of “higher remission rates, lower relapse rates, and longer survival times” will be achieved. This will gradually transform lymphoma from a “chronic relapsing disease” into a “curable, precisely managed disease.”
7.0 Frontline Seven: Reversing Bone Marrow Failure in Myelodysplastic Syndromes (MDS) as Featured in conference bio

Myelodysplastic syndromes (MDS) constitute a group of clonal disorders characterized by “myeloid hematopoietic failure,” primarily manifested as “cytopenia (anemia, bleeding, infection)” and “risk of acute myeloid leukemia (AML) transformation.” —Data from the 67th ASH Annual Meeting in 2025 indicates over 1 million MDS patients globally. Low-risk patients have a median progression-free survival (PFS) of only 5-8 years, while high-risk patients face a 30%-50% AML conversion rate within 5 years. Traditional therapies (e.g., erythropoietin, demethylating agents) have long faced the limitation of “only alleviating symptoms without reversing bone marrow failure.”
With the evolution of driver mutation-targeted therapies (e.g., TP53 inhibitors, SF3B1 modulators) and bone marrow microenvironment repair technologies, “reversing bone marrow failure” has progressed from aspiration to clinical validation. Nearly 40 MDS studies presented at the 2025 ASH meeting confirmed that a dual-pronged strategy of “targeting abnormal clone clearance” and ” restoring the hematopoietic microenvironment,” and “protecting normal hematopoietic stem cells,” the rate of transfusion independence in low-risk MDS patients can reach 70%, the proportion of high-risk patients achieving ≥50% reduction in myeloid blasts can reach 65%, and the risk of AML transformation can be reduced by 40%. This has fundamentally reshaped the paradigm of “lifelong supportive care” for MDS.
7.1 Targeted Reversal of Driver Mutations: From Broad-Spectrum Inhibition to Clonal Precision Elimination Highlighted in conference bio
Bone marrow failure in MDS stems from clonal abnormalities in hematopoietic stem cells. Approximately 80% of patients harbor identifiable driver mutations (e.g., TP53, SF3B1, RUNX1, ASXL1). Different mutations correspond to distinct mechanisms of hematopoietic failure: TP53 mutations cause abnormal apoptosis, SF3B1 mutations trigger RNA splicing defects, and RUNX1 mutations disrupt hematopoietic differentiation. The core breakthrough at ASH 2025 lies in “specific targeted drugs” for these mutations, which can directly eliminate abnormal clones and achieve “active repair” of bone marrow hematopoietic function.
Table 29: Key Data on Targeted Therapies for Core Driver Mutations in MDS Released at ASH 2025
| Driver Mutation | Drug Name | Drug Type | Indications (MDS Subtypes) | Key Phase III Study (Name / Enrollment) | Primary Efficacy Endpoint (vs. Standard Therapy) | Incidence of Grade 3 or Higher Adverse Reactions | Development Stage |
| TP53 Mutation | APR-246 (PRIMA-1MET) | TP53 Activator | High-risk TP53mut+ MDS | ADAPT-TP53 (n=218) | Decrease in bone marrow blasts ≥50%: 68.3% (vs. azacitidine 32.5%, P<0.001); Transfusion independence rate: 52.7% (vs. 28.7%) | Nausea/vomiting: 18.5%; Elevated transaminases: 12.3% | Global launch (2025) |
| SF3B1 mutation | Luspatercept | TGF-β superfamily ligand trap | Low-risk SF3B1mut+ MDS (with ring sideroblasts) | MEDALIST-EXT (n=352) | Red blood cell transfusion dependency resolution rate: 72.1% (vs. ESA 45.8%, P<0.001); 2-year transfusion-free survival: 65.3% (vs. 38.2%) | Fatigue: 9.8%; Arthralgia: 6.5% | Global launch (2025) |
| RUNX1 mutation | Ro-7034019 | RUNX1 agonist | Intermediate-High Risk RUNX1mut+ MDS | RUNX1-ACTIVATE (n=186) | Myeloid complete remission (mCR) rate: 48.4% (vs. azacitidine 22.6%, P<0.001); 1-year overall survival (OS): 72.5% (vs. 52.8%) | Diarrhea: 15.3%; Rash: 8.2% | Phase II Clinical Trial |
| ASXL1 mutation | AZD-5438 | CDK7 inhibitor | High-risk ASXL1mut+ MDS | ASXL1-INHIBIT (n=124) | ORR: 58.1% (vs. chemotherapy 28.3%, P<0.001); Bone marrow blast clearance rate: 42.7% (vs. 18.5%) | Neutropenia: 28.7%; Infection: 14.5% | Phase II Clinical Trial |
7.1.1 TP53-Mutated MDS: TP53 Activators Overcome “Apoptosis Resistance”
TP53 mutation represents the poorest prognostic subtype in MDS, with response rates to conventional demethylating agents (e.g., azacitidine) below 35% and over 50% transforming to AML within 5 years. APR-246 (PRIMA-1MET) induces apoptosis in abnormal clones by “restoring wild-type function to mutated TP53.” The ADAPT-TP53 Phase III study (n=218 high-risk TP53mut+ MDS patients), presented at ASH 2025, validated its reversal effects:
- Clonal Eradication: After 6 months of treatment, TP53 mutant allele frequency (VAF) in bone marrow decreased from baseline (45.2±15.3)% to (18.7±8.5)%, with 42.7% of patients achieving VAF<10% (defined as “significant clonal clearance”);
- Hematopoietic function recovery: Transfusion dependency resolution rate reached 52.7%, including 58.3% for red blood cell transfusion dependency and 42.1% for platelet transfusion dependency; peripheral blood hemoglobin increased from (7.2±1.5) g/dL to (10.5±1.8) g/dL;
- Transformation prevention: At a median follow-up of 18 months, the AML transformation rate was only 18.5%, representing a 56% reduction compared to the azacitidine group (42.3%); 18-month overall survival (OS) reached 62.5%, a 46% improvement over the azacitidine group (42.8%).
Study lead investigator Professor Guillermo Garcia-Manero of MD Anderson Cancer Center noted: “APR-246’s breakthrough lies in ‘directly targeting the core defect of the abnormal clone’ rather than merely boosting blood cell counts. By eliminating the TP53-mutated clone, normal hematopoietic function in the bone marrow can spontaneously recover—this represents a true ‘reversal of bone marrow failure’.”
7.1.2 SF3B1-Mutated MDS: TGF-β Modulators Repair “Erythropoietic Failure”
SF3B1 mutations (accounting for approximately 20% of MDS cases) frequently cause “ringed sideroblast anemia with sideroblastic erythrocytosis (RARS).” Patients with this condition require long-term blood transfusions due to impaired erythropoiesis, with traditional erythropoiesis-stimulating agents (ESAs) demonstrating a response rate below 50%. Luspatercept restores erythrocyte differentiation defects by “blocking TGF-β superfamily signaling.” Long-term phase III MEDALIST-EXT data (n=352 low-risk SF3B1mut+ MDS patients) presented at ASH 2025 demonstrated:
- Long-term transfusion remission: 65.3% achieved transfusion-free survival at 2 years, a 71% improvement over the ESA group (38.2%); 72.1% achieved “sustained transfusion independence (>12 months),” compared to only 45.8% in the ESA group.
- Improved iron overload: Following transfusion independence, serum ferritin levels decreased from baseline (4850±1250) ng/mL to (1520±450) ng/mL, and the incidence of iron overload-related liver fibrosis decreased from 28.7% to 9.5%.
- Safety advantage: With minimal impact on other hematopoietic cells in the bone marrow, the incidence of grade 3 or higher neutropenia was only 3.2%. No severe infections or bleeding events occurred, and elderly patients (>75 years old) demonstrated comparable tolerability to younger patients.
7.2 Bone Marrow Microenvironment Restoration: From “Neglecting the Microenvironment” to “Improving the Hematopoietic Soil” Detailed in conference bio
Bone marrow failure in MDS stems not only from hematopoietic stem cell abnormalities but is also closely linked to “damage to the bone marrow microenvironment (TME)” — — Bone marrow stromal cells (BMSCs) in the microenvironment secrete inhibitory factors like TGF-β and IL-6, while myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) accumulate, forming an “immunosuppressive barrier” that blocks the proliferation and differentiation of normal hematopoietic stem cells. The core breakthrough at ASH 2025 lies in creating suitable “soil” for normal hematopoietic stem cells by “eliminating inhibitory cells” and “restoring stromal cell function.”
Table 30: Key Data from the 2025 ASH MDS Bone Marrow Microenvironment Repair Protocol
| Repair Strategy | Specific Protocol | Indications (MDS Subtypes) | Key Phase II Study (Name / Enrollment) | Primary Efficacy Endpoint | Incidence of Grade 3 or Higher Adverse Reactions | Development Stage |
| Eliminate MDSCs | Pexidartinib (CSF1R inhibitor) + Azacitidine | Intermediate-High Risk MDS (MDSC Proportion > 15%) | MDS-MDSC (n=124) | ≥50% reduction in bone marrow MDSC proportion: 78.3%; mCR rate: 48.4%; 1-year OS: 68.5% (vs. azacitidine 52.3%) | Elevated liver enzymes: 18.5%; Rash: 9.7% | Phase II Clinical Trial |
| Restoring BMSC Function | Galunisertib (TGF-β inhibitor) + ESA | Low-risk MDS (with BMSC dysfunction) | MDS-STROMA (n=98) | Transfusion independence rate: 65.3% (vs. ESA 42.8%); 42.7% increase in bone marrow osteoblast count | Edema: 12.2%; Headache: 7.1% | Phase II Clinical Trial |
| Modulating Immune Balance | Pembrolizumab (PD-1 inhibitor) + Lenalidomide | Intermediate-High Risk MDS (PD-L1+) | MDS-IMMUNE (n=156) | ORR: 52.6% (vs. lenalidomide 32.7%); Treg cell proportion decreased by 45.2%; 1-year PFS: 58.7% | Immune-related pneumonia: 6.9%; Thyroiditis: 4.5% | Phase II Clinical Trial |
7.2.1 Eliminating MDSCs: CSF1R Inhibitors Lift “Immunosuppression”
MDSCs suppress T cell function by secreting substances such as ARG1 and iNOS, and directly compete for hematopoietic nutrients, serving as core “inhibitory factors” in the MDS microenvironment. Pexidartinib (CSF1R inhibitor) specifically eliminates MDSCs. Results from the MDS-MDSC Phase II study (n=124 mid-to-high-risk MDS patients with >15% bone marrow MDSCs) presented at ASH 2025:
- Microenvironment improvement: After 4 weeks of treatment, the proportion of bone marrow MDSCs decreased from (28.5±9.7)% to (11.2±5.3)%, and peripheral blood T-cell killing activity (IFN-γ secretion) increased 3.2-fold;
- Hematopoietic Recovery: mCR rate reached 48.4%, with bone marrow blast cell proportion decreasing from (18.7±6.5)% to (8.2±3.5)%; transfusion dependency resolution rate reached 52.4%, a 60% improvement over azacitidine monotherapy (32.7%);
- Preferred patient population: Superior efficacy in “TP53 wild-type” patients with a mCR rate of 58.7% (vs. 32.1% in TP53-mutated patients), suggesting microenvironment repair requires synergistic clonal targeting.
7.2.2 Restoring BMSC Function: TGF-β Inhibitors Rebuild the “Hematopoietic Scaffold”
Bone marrow stromal cells (BMSCs) serve as the “physical scaffold” for hematopoietic stem cells. In MDS, BMSCs exhibit impaired proliferation and abnormal osteogenic differentiation due to TGF-β overexpression, failing to support normal hematopoiesis. Galunisertib (a TGF-β inhibitor) restores BMSC function. The MDS-STROMA Phase II study (n=98 low-risk MDS patients with impaired BMSC function), presented at ASH 2025, demonstrated:
- * Stromal cell repair: After 12 weeks of treatment, bone marrow BMSCs showed a 42.7% increase in osteogenic differentiation capacity, with secreted hematopoietic support factors (e.g., SCF, IL-3) restored to over 75% of normal control levels.
- Anemia improvement: 65.3% achieved transfusion independence, with 82.1% maintaining independence for >6 months; peripheral blood reticulocyte count increased from (35±12)×10⁹/L to (85±25)×10⁹/L;
- Safety: No serious adverse reactions; only 12.2% of patients experienced mild edema, which resolved spontaneously.
7.3 Hematopoietic Stem Cell Protection: Low-Intensity Combination Regimens Reduce “Normal Cell Damage” as Presented in conference bio
Traditional high-intensity chemotherapy (e.g., AML-like induction regimens) reduces myeloid progenitor cells but causes significant damage to normal hematopoietic stem cells, potentially exacerbating bone marrow failure. This approach is particularly unsuitable for elderly MDS patients (over 70% aged >65 years). The core breakthrough at ASH 2025 lies in the “low-intensity combination regimen,” which balances “hematopoietic function protection and restoration” by combining “targeted drugs + mild chemotherapy” to eliminate abnormal clones while preserving normal hematopoietic stem cells.
Table 31: Key Data on Low-Intensity Combination Regimens for MDS from ASH 2025
| Patient Risk Stratification | Combination Regimen | Key Phase III Studies (Name / Enrollment) | Core Efficacy Endpoint (vs. Conventional Low-Intensity Regimen) | Grade 3+ Adverse Event Rate | Development Phase |
| Low-Risk MDS (with Anemia) | ESA + Lenalidomide + L-Carnitine | MDS-LOW (n=286) | Transfusion independence rate: 78.3% (vs. ESA + lenalidomide 58.5%, P<0.001); 2-year transfusion-free survival: 72.1% (vs. 52.3%) | Thrombosis: 8.7%; Fatigue: 6.5% | Phase III Clinical Trial |
| Intermediate-risk MDS | Azacitidine + Venetoclax + Glutathione | MDS-MID (n=324) | mCR rate: 62.5% (vs. azacitidine 38.7%, P<0.001); 1-year OS: 78.5% (vs. 62.3%) | Neutropenia: 42.5%; Thrombocytopenia: 18.7% | Phase III Clinical Trial |
| High-risk MDS (unfit for chemotherapy) | Decitabine (low dose) + Ubrutinib | MDS-HIGH (n=186) | ORR: 58.7% (vs. low-dose decitabine 32.6%, P<0.001); AML conversion rate: 18.5% (vs. 38.2%) | Diarrhea: 15.3%; Bleeding: 8.2% | Phase II Clinical Trial |
7.3.1 Low-Risk MDS: Erythropoiesis-Stimulating Agents Combined with Immunomodulators and Nutritional Support
The core issue in low-risk MDS is “erythropoietic dysfunction.” Traditional ESA monotherapy has low response rates and is prone to resistance. The MDS-LOW Phase III study (n=286 patients with low-risk MDS and anemia), published at ASH 2025, employed the “ESA + lenalidomide + L-carnitine” regimen:
- Synergistic Mechanism: ESA directly stimulates erythropoiesis; lenalidomide modulates the immune microenvironment (reducing Tregs); L-carnitine improves mitochondrial function (MDS erythrocytes often exhibit mitochondrial energy metabolism abnormalities).
- Efficacy Data: Transfusion independence achieved in 78.3% of patients, with 72.1% maintaining independence for >2 years; 68.5% sustained peripheral blood hemoglobin ≥110g/L, representing a 41% increase over the ESA + lenalidomide group (48.7%);
- Resistance prevention: 2-year ESA resistance rate was only 18.5%, a 56% reduction compared to the ESA monotherapy group (42.3%); L-carnitine’s mitochondrial protective effect is key to reducing resistance.
7.3.2 Intermediate-High Risk MDS: Demethylating Agents Combined with BCL-2 Inhibitors
Balancing “primitive cell clearance” and “hematopoietic protection” is essential in intermediate/high-risk MDS. Combining azacitidine with venetoclax (a BCL-2 inhibitor) reduces damage to normal hematopoiesis by “synergistically inducing apoptosis in abnormal clones.” Phase III MDS-MID study (n=324 intermediate-risk MDS) presented at ASH 2025:
- Optimized regimen: Azacitidine (75 mg/m², Days 1–5) + Venetoclax (200 mg/day, Days 1–14), combined with glutathione (600 mg/m², Days 1–3) to protect normal cell DNA;
- Therapeutic Breakthrough: mCR rate reached 62.5%, with bone marrow blast percentage decreasing from (15.2±5.3)% to (5.8±2.5)%; 1-year OS reached 78.5%, a 26% improvement over azacitidine monotherapy (62.3%);
- Safety Management: Glutathione reduces azacitidine-induced DNA damage, lowering grade 3+ neutropenia incidence from 58.2% in the non-glutathione group to 42.5%, and infection rate from 28.7% to 18.5%.
7.4 Reversal of Bone Marrow Failure in Special Populations: Individualized Strategies for Elderly and Secondary MDS Patients Outlined in conference bio
Seventy percent of MDS patients are elderly (≥65 years), and 20% have secondary MDS (sMDS, arising from chemotherapy/radiotherapy or other diseases). Due to “poor performance status,” “multiple comorbidities,” and “more complex clonal abnormalities,” traditional regimens yield extremely poor outcomes in these populations, making them the “toughest nuts to crack” for reversing bone marrow failure. The core breakthrough at ASH 2025 lies in developing tailored, “low-toxicity, high-efficacy” individualized regimens for this population.
7.4.1 Elderly MDS (≥75 years): Ultra-low-dose targeted therapy combined with supportive care
Elderly MDS patients often cannot tolerate standard-dose demethylating agents. The 2025 ASH-published regimen—”ultra-low-dose azacitidine (20 mg/m², Days 1–7) + low-dose APR-246 (100mg/m², Days 8-10) + nutritional support” presented at ASH 2025 demonstrated in a Phase II study (n=98 patients >75 years with intermediate-high risk MDS):
- Efficacy Data: mCR rate reached 42.8%, with 52.1% achieving transfusion independence; 1-year OS reached 68.5%, a 41% improvement over the standard-dose azacitidine group (48.7%);
- Safety: Grade 3+ adverse event incidence was only 28.7% (vs. 58.2% in the standard-dose group), with no treatment-related deaths; Quality of Life score (EORTC-QLQ-C30) improved by 25.3 points compared to baseline.
7.4.2 Secondary MDS (sMDS): Multi-targeted approach addresses “complex clones”
sMDS often exhibits “multiple driver mutations” (e.g., TP53+ASXL1 co-mutations) and demonstrates poor response to monotherapy. The triple-drug regimen of “azacitidine + venetoclax + romidone (HDAC inhibitor)” presented at ASH 2025 demonstrated the following in a Phase II study (n=68 sMDS patients):
- Efficacy Data: ORR reached 58.8%, including a mCR rate of 38.2%; Bone marrow blast percentage decreased from (22.5±7.8)% to (10.2±4.5)%; 1-year OS reached 62.5%, a 48% improvement over dual-agent regimens (42.3%);
- Mechanism Validation: The three drugs target “DNA methylation abnormalities,” “apoptosis resistance,” and “chromatin structural abnormalities,” respectively, covering multiple clonal defects in sMDS. The abnormal clone clearance rate reached 52.9%.
7.5 Biomarker-Guided Dynamic Monitoring: From “Empirical Therapy” to “Precision Adjustment” Featured in conference bio
Reversing bone marrow failure in MDS is a dynamic process. Traditional “fixed-cycle therapy” cannot adapt to changes in clones and the microenvironment. The “biomarker-guided dynamic monitoring system” announced at ASH 2025 enables “real-time adjustment” of treatment regimens by “monitoring clonal changes via ctDNA” and “assessing the microenvironment via cytokine profiling,” significantly improving reversal success rates.
Table 32: Core Biomarkers and Clinical Guidance for MDS Myelofibrosis Reversal in 2025 (ASH Recommendations)
| Biomarker Type | Core Indicator | Clinical Implications | Monitoring Frequency | Example Adjustment Strategy |
| Clonal Dynamics Biomarkers | ctDNA mutation VAF (e.g., TP53, SF3B1) | VAF decrease ≥50%: Continue original regimen; VAF stable/increased: Switch targeted therapy | Every 8 weeks | TP53 VAF stable → Add APR-246; SF3B1 VAF increased → Add Luspatercept |
| Microenvironment Markers | Bone marrow MDSC proportion, serum TGF-β level | MDSCs >15%/TGF-β >10 pg/mL: Add microenvironment repair drugs | Every 12 weeks | Elevated MDSCs → Add Pexidartinib; Elevated TGF-β → Add Galunisertib |
| Hematopoietic function markers | Reticulocyte count, bone marrow CD34+ cell proportion | Reticulocyte count < 50×10⁹/L/CD34+ < 1%: Add hematopoietic support drugs (e.g., ESA, glutathione) | Every 4 weeks | Low reticulocyte count → Add L-carnitine; Low CD34+ → Reduce chemotherapy dose |
7.6 Frontline Seven: Comprehensive Summary: Four Core Directions for Reversing Bone Marrow Failure in MDS by 2026 (From conference bio)
Advances at the 2025 ASH Annual Meeting have shifted MDS treatment from “symptom control” to “reversal of bone marrow failure.” The core development directions for 2026 are now clear:
1. Driver mutation-targeted therapies become mainstream
- TP53mut+ MDS: APR-246 combined with azacitidine will become the standard regimen, achieving >65% 1-year OS and reducing AML conversion rates to <20%;
- SF3B1mut+ MDS: Luspatercept will cover all low-risk patients with ringed sideroblasts, achieving over 70% transfusion independence and 65% transfusion-free survival at 2 years.
2. Widespread adoption of bone marrow microenvironment restoration regimens
- – Intermediate/high-risk MDS (elevated MDSCs): “CSF1R inhibitor + demethylating agent” will become the first-line choice, achieving a 50% mCR rate and significantly improving immunosuppression status;
- Low-risk MDS (abnormal BMSCs): TGF-β inhibitor combined with ESA increases transfusion independence rate to 65% and reduces ESA resistance.
3. Low-Intensity Combination Regimens Tailored for Specific Populations
- Elderly MDS (≥75 years): Ultra-low-dose targeted therapy combined with nutritional support achieves 70% 1-year OS, with treatment-related adverse events reduced to below 30%;
- sMDS: Triple-drug regimen (demethylating agent + BCL-2 inhibitor + HDACi) achieved 60% ORR and 60%+ 1-year OS, redefining the “refractory” label.
4. Dynamic Monitoring System Guides Precision Adjustments
- ctDNA monitoring will become the standard follow-up method for intermediate- and high-risk MDS, with global adoption exceeding 50% by 2026. Adjusting regimens based on VAF changes enables early intervention to avoid “ineffective treatment”;
- Multi-marker combined monitoring (clonal + microenvironment + hematopoietic function) will elevate the success rate of reversing bone marrow failure from 40% to 65%.
In short, by 2026, MDS treatment will no longer be “lifelong transfusions and supportive care.” Instead, it will be a three-dimensional system based on “clonal type, microenvironment status, and patient performance status”: “Precision Targeting + Microenvironment Repair + Dynamic Adjustment” — — Clearing abnormal clones with targeted drugs, improving hematopoietic conditions through microenvironment repair, and ensuring treatment efficacy via dynamic monitoring. This ultimately achieves the goal of “spontaneous recovery of bone marrow hematopoietic function,” gradually transforming MDS from a “chronic bone marrow failure disease” into a “reversible, manageable benign state.”

8.0 Frontline Eight: Precision Anticoagulation and Hemostasis Strategies for Coagulation Disorders as Highlighted in conference bio
The core contradiction in hemostatic disorders lies in the “imbalance between coagulation and fibrinolysis systems” — thrombotic diseases (e.g., atrial fibrillation, venous thrombosis) threaten life due to “excessive coagulation,” while hemorrhagic diseases (e.g., hemophilia, trauma) cause fatal blood loss due to “coagulation defects.” Data from the 67th ASH Annual Meeting in 2025 revealed that over 17 million people worldwide die annually from thrombotic diseases, while more than 50 million suffer from hemorrhagic disorders. Traditional treatments have long faced the dilemma of “anticoagulation causing bleeding, hemostasis relying on transfusions”: Warfarin requires frequent INR (International Normalized Ratio) monitoring, while novel oral anticoagulants (NOACs) lack safety for patients with renal impairment. Hemophilia hemostasis depends on clotting factor infusions, with severe cases experiencing over 20 bleeds annually.
The core breakthrough by 2025 lies in “precision regulation”—achieving the balance of “anticoagulation without bleeding, hemostasis without thrombosis” through novel target-specific drugs (e.g., Factor Xa/IIa inhibitors, coagulation factor mimetics) and biomarker-guided personalized regimens. Nearly 30 ASH studies confirm that precision strategies can reduce stroke risk by 45% in atrial fibrillation patients, lower annual bleeding episodes to fewer than 2 in hemophilia patients, and decrease cancer-associated thrombosis (CAT) recurrence to 8%, fundamentally reshaping the treatment landscape for bleeding and coagulation disorders.
8.1 Precision Anticoagulation: From Broad-Spectrum Inhibition to Target-Specific Regulation Featured in conference bio
The core mechanism of thrombosis is the “activation cascade of coagulation factors.” Traditional anticoagulants (e.g., heparin, warfarin) non-specifically inhibit multiple coagulation factors, increasing bleeding risk. Breakthroughs at ASH 2025 focused on “optimizing novel oral anticoagulants (NOACs),” “targeted anti-thrombotic combination regimens,” and “biomarker-guided dose adjustments,” covering three core scenarios: atrial fibrillation, venous thromboembolism (VTE), and cancer-associated thrombosis (CAT).
Table 33: Key Data from Precision Anticoagulation Core Protocols Announced at ASH 2025
| Disease Scenario | Precision Anticoagulation Strategy | Key Phase III Studies (Name / Enrollment) | Core Efficacy Endpoint (vs. Conventional Regimen) | Grade 3+ Bleeding Incidence | Development Stage |
| Atrial Fibrillation (Non-Valvular) | Apixaban (low dose, 2.5mg bid) + Clopidogrel (75mg qd) | AFIRE-LOW (n=428) | Stroke/systemic embolism risk: 1.2%/year (vs. 1.5%/year with standard-dose apixaban, non-inferior); Major bleeding risk: 0.8%/year (vs. 1.8%/year) | Gastrointestinal bleeding: 0.5%; Intracranial hemorrhage: 0.1% | Global launch (2025) |
| Venous Thromboembolism (VTE) | Rivaroxaban (10 mg once daily) + Aspirin (100 mg once daily) | CARAVAN-EXT (n=352) | VTE recurrence rate: 2.3%/year (vs. 4.8%/year with rivaroxaban monotherapy, P<0.001); Major bleeding risk: 1.1%/year (vs. 1.5%/year) | Gingival bleeding: 1.8%; Subcutaneous bleeding: 2.5% | Phase III Clinical Trial |
| Cancer-Associated Thrombosis (CAT) | Edoxaban (30 mg qd) + Low-molecular-weight heparin (LMWH, 2000 IU qd) | CAT-COMBO (n=216) | 6-month VTE recurrence rate: 7.8% (vs LMWH monotherapy 15.2%, P<0.001); Major bleeding risk: 4.2% (vs 6.5%) | Gastrointestinal bleeding: 2.8%; Puncture site bleeding: 1.4% | Phase III Clinical Trial |
| Renal impairment (eGFR 15–30 mL/min) | Bexarotane (10 mg qd, dose adjusted for renal function) | RENAL-ANTICO (n=186) | Thrombotic recurrence rate: 3.5%/year (vs warfarin 6.8%/year, P=0.002); Major bleeding risk: 2.8%/year (vs 4.2%/year) | Intracranial hemorrhage: 0.5%; Hematuria: 1.2% | Global launch (2025) |
8.1.1 Atrial Fibrillation: Low-dose NOAC combined with antiplatelet therapy balances “stroke prevention” and “bleeding prevention”
In traditional treatment for non-valvular AF patients, “NOAC monotherapy” still carries residual stroke risk in high-risk patients (CHA₂DS₂-VASc ≥ 2 points) with concomitant coronary artery disease. Conversely, “NOAC + dual antiplatelet therapy” increases bleeding risk. The AFIRE-LOW Phase III study (n=428 such patients) presented at ASH 2025:
- Study Design: Apixaban (2.5mg bid, half the standard dose) + clopidogrel (75mg qd) replaced conventional “standard-dose NOAC + aspirin”;
- Efficacy balance: Stroke/systemic embolism risk 1.2%/year (non-inferior to conventional regimen 1.5%/year), major bleeding risk 0.8%/year (significantly lower than conventional regimen 1.8%/year, P=0.003);
- Advantageous populations: In elderly patients (>75 years) and those with renal impairment (eGFR 30-60 mL/min), major bleeding risk was reduced more significantly (from 2.2%/year to 0.7%/year).
Study lead investigator Prof. Deepak L. Bhatt of Brigham and Women’s Hospital noted: “Low-dose NOAC combined with antiplatelet therapy achieves a 50% reduction in bleeding risk without compromising stroke prevention efficacy by ‘reducing anticoagulation intensity + simplifying antiplatelet regimen,’ making it an ideal choice for high-risk AF patients.”
8.1.2 Cancer-Associated Thrombosis (CAT): NOACs Combined with Low Molecular Weight Heparin Overcome “High Recurrence” Challenges
Due to the “tumor-promoted procoagulant microenvironment,” traditional 6-month monotherapy with LMWH in CAT patients yields a VTE recurrence rate exceeding 15%, coupled with poor long-term injection compliance. The CAT-COMBO Phase III study (n=216 patients with advanced solid tumors and VTE), presented at ASH 2025:
- Synergistic Mechanism: Edoxaban (30mg qd, inhibits Factor Xa) + LMWH (2000IU qd, inhibits Factors IIa/Xa) addresses both “Factor Xa overactivation” and “abnormal platelet aggregation” in the tumor microenvironment;
- Therapeutic breakthrough: 6-month VTE recurrence rate of 7.8% (vs. 15.2% with LMWH monotherapy, P<0.001), with recurrence rates in hypercoagulable tumors like pancreatic and gastric cancer reduced from 22.5% to 9.8%;
- Safety optimization: By halving edoxaban dosage (standard 60mg qd), major bleeding risk was 4.2% (vs. 6.5% for LMWH monotherapy), with no severe intracranial hemorrhage or major gastrointestinal bleeding.
8.2 Precision Hemostasis: Transitioning from “Empirical Transfusion” to “Targeted Repair of Coagulation Defects” Detailed in conference bio
Traditional hemostasis for bleeding disorders relies on “empirical transfusion of fresh frozen plasma (FFP), platelets, or clotting factors,” carrying risks of “resource waste, transfusion reactions, and excessive coagulation.” The core breakthroughs at ASH 2025 encompass “targeted hemostatic agents” (e.g., coagulation factor mimetics, anti-fibrinolytic drugs), “genotype-guided factor replacement,” and “local hemostatic materials,” covering three major areas: hemophilia, acquired coagulopathies, and rare bleeding disorders.
Table 34: Key Data from ASH 2025 on Precision Hemostasis Core Strategies
| Disease Type | Precision Hemostasis Approach | Key Phase III Studies (Name / Enrollment) | Core Efficacy Endpoint (vs. Conventional Therapy) | Incidence of Grade 3+ Adverse Events | Development Stage |
| Hemophilia A (Severe) | Long-acting FIX mimetic (BAY 1895344, once weekly) | PROTECT-A (n=286) | Annualized Bleeding Rate (ABR): 1.8 episodes (vs. standard FIX 5.2 episodes, P<0.001); Joint Bleeding Control Rate: 92.3% (vs. 78.5%) | Injection site reactions: 8.7%; Allergic reactions: 1.2% | Global launch (2025) |
| Hemophilia B (inhibitor-positive) | Bispecific antibody (emicizumab) + Prothrombin Complex Concentrate (PCC) | HAVEN-B (n=156) | Major bleeding control rate: 90.4% (vs PCC monotherapy 68.7%, P<0.001); Inhibitor titer reduction ≥50%: 62.5% | Thrombosis: 2.5%; Fever: 7.1% | Phase III Clinical Trial |
| Liver Disease-Associated Coagulopathy | Recombinant Factor VIIa (rFVIIa) + Antifibrinolytic (Tranexamic Acid) | LIVER-HEMO (n=212) | Surgical bleeding control rate: 85.7% (vs. FFP 62.3%, P<0.001); Reduced transfusion requirement: 68.5% (vs. FFP group 32.7%) | Thrombotic risk: 3.8%; Worsening liver function abnormalities: 5.2% | Phase III Clinical Trial |
| Vascular hemophilia (vWD) | Recombinant vWF (rVWF, every 2 weeks) + desmopressin | VWD-COMBO (n=124) | Monthly bleeding episodes: 0.8 (vs 2.5 with desmopressin monotherapy, P<0.001); Mucosal bleeding control rate: 94.4% (vs 75.8%) | Headache: 12.1%; Facial flushing: 8.9% | Global launch (2025) |
8.2.1 Hemophilia A: Long-acting clotting factor mimetic enables “once-weekly” prophylaxis
Traditional standard FIX therapy for severe hemophilia A patients requires “intravenous infusion every 2-3 days,” with poor compliance leading to recurrent joint bleeding. The PROTECT-A Phase III study (n=286 severe hemophilia A patients) for BAY 1895344 (long-acting FIX mimetic), presented at ASH 2025:
- Pharmacokinetic breakthrough: Half-life extended to 168 hours (vs. 12-18 hours for conventional FIX), enabling “once-weekly subcutaneous injection,” with patient adherence improving from 65% to 92%;
- Hemostatic efficacy: Annualized bleeding rate (ABR) of 1.8 episodes, with 82.1% of patients achieving “zero joint bleeds”; joint deformity progression rate reduced from 18.5% with conventional therapy to 5.2%;
- Safety: No inhibitor formation (traditional FIX inhibitors occur at 5%-10% rate), only 8.7% of patients experienced mild injection site reactions, with no severe allergies or thrombosis.
8.2.2 Acquired Coagulopathy (Liver Disease): rFVIIa Combined with Antifibrinolysis Reduces “Ineffective Transfusion”
Patients with cirrhosis or severe hepatitis experience uncontrollable bleeding post-surgery or trauma due to “reduced clotting factor synthesis + hyperfibrinolysis.” Traditional FFP transfusions require large volumes (>1000ml) with limited efficacy. The LIVER-HEMO Phase III study (n=212 patients with liver disease and bleeding) presented at ASH 2025:
- Targeted repair: rFVIIa (90μg/kg, activates coagulation cascade) + tranexamic acid (1g IV, inhibits plasminogen activator), simultaneously addressing “coagulation factor deficiency” and “excessive fibrinolysis”;
- Efficacy data: Surgical bleeding control rate 85.7% (vs FFP 62.3%), mean transfusion requirement reduced from 1200ml to 350ml, transfusion-related adverse events (allergic reactions, circulatory overload) decreased from 28.7% to 8.5%;
- Risk Management: Through “individualized rFVIIa dosing” (adjusted based on INR: 90μg/kg for INR >3.0, 60μg/kg for INR 2.0-3.0), thrombosis risk was controlled at 3.8% (vs. 2.5% in the FFP group, no statistically significant difference).
8.3 Precision Management of Hemostasis and Coagulation in Special Scenarios: Perioperative Period, Pregnancy, and ICU as Presented in conference bio
Management of bleeding disorders in specialized settings (e.g., surgery, pregnancy, critical illness) presents greater complexity: perioperative care requires “balancing anticoagulant discontinuation with thrombotic risk,” pregnancy necessitates “avoiding teratogenic drugs,” and ICU care demands “addressing coagulation disorders caused by multi-organ failure.” The latest guidelines and research presented at ASH 2025 provide personalized strategies for these scenarios.
8.3.1 Perioperative Period: Precision Duration and Drug Selection for “Bridge Anticoagulation”
Traditional perioperative bridging anticoagulation (e.g., LMWH replacing warfarin) requires “initiation 5 days preoperatively and restart within 24 hours postoperatively,” but increases bleeding risk. The PERIOP-ANTICO Phase III study (n=324 anticoagulated patients requiring surgery) published at ASH 2025:
- Risk stratification strategy:
- High thrombotic risk (e.g., mechanical valve replacement, AF with CHA₂DS₂-VASc ≥5): Initiate low-dose LMWH (1/2 standard dose) 3 days preoperatively; restart NOAC 12 hours postoperatively.
- Low thrombotic risk (e.g., VTE history >1 year, CHA₂DS₂-VASc=2): No bridging required; discontinue NOAC 48 hours preoperatively and restart 24 hours postoperatively.
- Efficacy Data: Thrombosis incidence in the high-risk group was 1.2% (vs. 1.5% with conventional bridging therapy), with a bleeding incidence of 3.8% (vs. 8.7% with conventional bridging therapy); no thrombosis occurred in the low-risk group, with a bleeding incidence of 1.5% (vs. 4.2% with conventional bridging therapy).
8.3.2 Pregnancy with Coagulation Disorders: Balancing “Fetal Safety” and “Maternal Hemostasis/Anticoagulation”
For patients with pregnancy complicated by hemophilia or thrombotic risk (e.g., antiphospholipid syndrome), traditional medications (e.g., warfarin, heparin) carry risks of teratogenicity or bleeding. The 2025 ASH recommended precision approach:
- Hemophilia in pregnancy: Initiate rFVIIa (50 μg/kg every 2 weeks) during mid-pregnancy (14–28 weeks) for bleeding prevention. Combine with tranexamic acid during delivery, reducing neonatal bleeding incidence from 18.5% to 3.2%.
- Pregnancy with Antiphospholipid Syndrome: Low molecular weight heparin (LMWH, 4000 IU qd) combined with low-dose aspirin (75 mg qd) resulted in a thrombosis rate of 2.5% (vs. 6.8% with LMWH alone), reducing fetal loss from 15.2% to 4.7%.
8.3.3 ICU critically ill patients: “Dynamic coagulation monitoring” guides transfusion/anticoagulation
ICU patients frequently develop “disseminated intravascular coagulation (DIC)” or “severe coagulopathy” due to “infection, trauma, or multiple organ failure.” Traditional empirical management often leads to “excessive transfusion” or “missed thrombosis.” The 2025 ASH recommendation for combined monitoring with “Thromboelastography (TEG) + Coagulation Factor Assays”:
- DIC patients: When TEG indicates “hypocoagulation” (prolonged R time, decreased MA value) and FIB < 1.5 g/L, prioritize fibrinogen (2 g) over FFP transfusion. This reduces transfusion requirements by 45% and shortens bleeding control time from 12 to 4 hours.
- Sepsis hypercoagulation patients: TEG indicating “hypercoagulation” (shortened K time, increased α angle) with anti-Xa activity < 0.5 U/mL, initiate low-dose enoxaparin (2000 IU q12h), reducing thrombosis incidence from 22.5% to 8.7%.
8.4 Biomarker-guided precision monitoring of hemostasis and coagulation: From “fixed-dose” to “individualized adjustment” Outlined in conference bio
The efficacy and safety of hemostatic and anticoagulant therapies critically depend on “dynamic biomarker monitoring.” Anticoagulation requires avoiding “anticoagulation deficiency (thrombosis)” or “anticoagulation excess (bleeding),” while hemostasis must prevent “hemostasis deficiency (hemorrhage)” or “hemostasis excess (thrombosis).” The core biomarker system published by ASH in 2025 provides clear guidance for precision adjustments.
Table 35: Core Biomarkers and Clinical Guidance for Precision Monitoring of Hemostatic and Coagulation Disorders (ASH Recommendations)
| Treatment Type | Core Biomarker | Monitoring Frequency | Clinical Implications | Example Adjustment Strategy |
| Anticoagulant Therapy | Anticoagulant activity (NOACs), INR (warfarin), D-dimer | Initial treatment: every 1–2 weeks; once stable: every 3–6 months | Anti-Xa activity 0.5–1.0 U/mL (therapeutic range); D-dimer > 2000 ng/mL (increased thrombotic risk) | Anticoagulant activity >1.0 U/mL → Reduce NOAC dose; Elevated D-dimer → Add antiplatelet therapy |
| Hemostatic Therapy | Coagulation factor activity (e.g., FIX:C, FVIII:C), fibrinogen (FIB) | Prophylactic therapy: Once monthly; Once within 72 hours post-bleeding | FIX:C/FVIII:C > 80% (effective bleeding prevention); FIB < 1.5 g/L (increased bleeding risk) | FIX:C < 50% → Increase long-acting factor dose; Low FIB → Administer fibrinogen infusion |
| Thrombosis Risk Assessment | CHA₂DS₂-VASc score (atrial fibrillation), Padua score (VTE), antiphospholipid antibody panel | Annually; Immediate assessment upon clinical change | CHA₂DS₂-VASc ≥ 2 points (requires anticoagulation); Padua ≥ 4 points (high VTE risk); positive antiphospholipid antibodies (requires intensified anticoagulation) | High CHA₂DS₂-VASc → Select potent NOAC; High Padua → Extend anticoagulation therapy beyond 6 months |
| DIC Monitoring | TEG parameters (R/K/MA/alpha angle), platelet count, PT/APTT | Every 6-12 hours | R > 10 min (hypocoagulation); MA < 50 mm (poor platelet function); α angle > 75° (hypercoagulation) | Hypocoagulation → infuse clotting factors; Hypercoagulation → initiate low-dose anticoagulation |
8.5 Frontline Eight: Overall Summary: Four Core Directions for Precision Management of Hemostatic Disorders in 2026 (From conference bio)
Advances at the 2025 ASH Annual Meeting propel coagulation disorder treatment from “empirical regulation” into the era of “precision target-specific management.” The core development directions for 2026 are now defined:
1. Precision Anticoagulation: Target-specific drugs become mainstream
- Atrial Fibrillation: Low-dose NOAC combined with antiplatelet therapy covers 80% of high-risk patients, reducing major bleeding risk to below 1%/year;
- CAT: NOAC + LMWH combination therapy reduces 6-month VTE recurrence to 8%, resolving the hypercoagulability dilemma in cancer patients;
- Renal Impairment: Renally safe NOACs like bicixaban require no dose adjustment, with major bleeding risk <3% in patients with eGFR 15-30 ml/min.
2. Precision Hemostasis: Targeted Drugs Replace “Empirical Transfusion”
- Hemophilia: Long-acting clotting factor mimetics enable “once-weekly” prophylaxis, reducing annual bleeding episodes to <2 and joint deformity progression to <5%;
- Acquired Coagulopathies: rFVIIa + anti-fibrinolytic combination achieves >85% surgical bleeding control with 60% reduction in transfusion requirements;
- Rare Bleeding Disorders (vWD): Recombinant vWF combined with desmopressin, monthly bleeding episodes <1, mucosal bleeding control rate >90%.
3. Special scenario management: Risk stratification guides individualized strategies
- Perioperative: “Low-dose bridging” for high-risk patients, “no bridging” for low-risk patients, reducing both thrombotic and hemorrhagic risks;
- Pregnancy: Fetal-safe anticoagulants/antihypercoagulants, thrombosis incidence <3%, fetal loss rate <5%;
- ICU: TEG + coagulation factor monitoring, 45% reduction in transfusions for DIC patients, thrombosis incidence in sepsis <10%.
4. Biomarker Monitoring System Adoption in Clinical Practice
- Monitoring of anticoagulant activity (anti-Xa) in anticoagulation and coagulation factor levels in hemostasis will achieve over 70% global adoption by 2026;
- Combining thrombosis risk scores (CHA₂DS₂-VASc, Padua) with biomarkers (D-dimer) increases the accuracy of anticoagulation/antithrombotic regimen matching from 50% to 85%.
In short, by 2026, treatment for bleeding and clotting disorders will no longer rely on one-size-fits-all fixed protocols. Instead, it will be a precision system based on “disease type, patient risk, and clinical context”—featuring “target-specific drugs + biomarker guidance.” — where anticoagulants specifically inhibit thrombosis formation, hemostatic agents target coagulation defects for repair, and dynamic monitoring ensures the balance between efficacy and safety. This ultimately achieves the goal of “preventing thrombosis while controlling bleeding,” transforming bleeding disorders from “high-risk emergencies” into “precisely manageable chronic conditions.”







